Understanding Meningitis and Its Symptoms
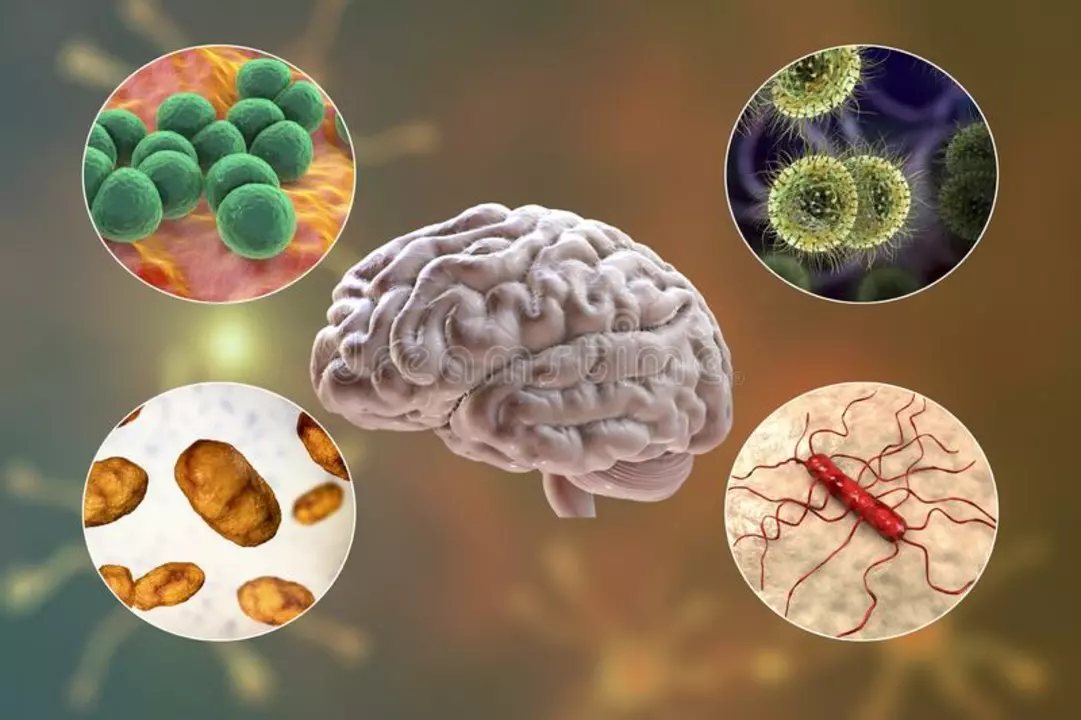
Meningitis is a serious medical condition that occurs when the protective membranes surrounding the brain and spinal cord, known as the meninges, become inflamed. This inflammation can be caused by a variety of factors, including bacterial, viral, and fungal infections. The symptoms of meningitis can vary greatly depending on the cause, but some common signs include fever, headache, neck stiffness, and sensitivity to light. In more severe cases, meningitis can lead to seizures, coma, and even death if left untreated.
It's crucial to recognize these symptoms early, as prompt treatment can mean the difference between life and death. If you suspect that you or someone you know may have meningitis, it's important to seek medical attention right away. In this article, we'll discuss the role of chloramphenicol, a powerful antibiotic, in the treatment of meningitis, as well as the potential risks and benefits of using this medication.
Chloramphenicol: A Potent Weapon Against Bacterial Infections
Chloramphenicol is a broad-spectrum antibiotic that has been used for decades to treat a wide range of bacterial infections. It works by inhibiting the production of essential proteins that bacteria need to survive and reproduce. This makes it a highly effective tool in the fight against many types of bacteria, including those that cause meningitis.
While there are several different types of meningitis, bacterial meningitis is generally considered the most dangerous. This is because it can progress rapidly and lead to serious complications if not treated promptly. In these cases, chloramphenicol can be a lifesaving medication, as it is able to penetrate the blood-brain barrier and attack the bacteria directly where they are causing damage.
When Chloramphenicol is the Best Option for Meningitis Treatment
While there are other antibiotics available for the treatment of meningitis, chloramphenicol is often the drug of choice in certain situations. One such scenario is when the specific bacteria causing the infection have not yet been identified. In these cases, chloramphenicol's broad-spectrum activity makes it a good option, as it is effective against a wide range of bacterial species.
Another situation where chloramphenicol may be the best choice for meningitis treatment is when the patient has an allergy to other antibiotics, such as penicillin or cephalosporins. In these cases, chloramphenicol can be a safe and effective alternative. However, it's important to note that chloramphenicol can also cause allergic reactions in some patients, so it's essential to discuss any known allergies with your healthcare provider before starting treatment.
Potential Risks and Side Effects of Chloramphenicol
While chloramphenicol can be an effective treatment for meningitis, it's important to be aware of the potential risks and side effects associated with this medication. Some of the most common side effects include nausea, vomiting, diarrhea, and changes in appetite. These side effects are generally mild and can be managed with proper care and attention.
However, there are also some more serious risks associated with chloramphenicol use. One of the most concerning is the potential for bone marrow suppression, which can lead to a decrease in the production of blood cells. This can result in an increased risk of infection, anemia, and bleeding problems. In rare cases, chloramphenicol can also cause a potentially fatal condition called aplastic anemia, which is characterized by the inability of the bone marrow to produce blood cells. It's crucial to monitor patients closely for any signs of bone marrow suppression while they are taking chloramphenicol.
Monitoring and Adjusting Treatment for Optimal Results
When a patient is being treated for meningitis with chloramphenicol, it's essential to closely monitor their progress and adjust treatment as needed. This may involve regular blood tests to check for signs of bone marrow suppression, as well as monitoring for any potential side effects. Depending on the patient's response to treatment, it may be necessary to adjust the dosage of chloramphenicol or to consider alternative antibiotics if the risks are deemed too great.
In conclusion, chloramphenicol can be a highly effective treatment for meningitis in certain situations. However, it's essential to weigh the potential risks and benefits carefully and to closely monitor patients during treatment to ensure the best possible outcome. As with any medical treatment, it's important to work closely with your healthcare provider to determine the most appropriate course of action for your specific situation.


Gary O'Connor
April 27, 2023 AT 01:17Looks like chloramphenicol’s still a go-to when you cant pin down the bug.
Justin Stanus
April 28, 2023 AT 10:37Chloramphenicol does the job when you’re in a bind, but it ain’t without its shadows. The blood‑brain barrier bypass is a real plus, especially if you’re waiting on cultures. Still, the bone‑marrow warning looms large – you don’t want to trade one nightmare for another. In practice, it’s a trade‑off that docs have to weigh every single time.
Claire Mahony
April 28, 2023 AT 13:24You make a solid point about the trade‑off; the risk of aplastic anemia can’t be brushed aside. Clinicians often run baseline CBCs and keep a tight watch, which mitigates surprises. It’s also worth noting that alternative agents may not cross the barrier as well, leaving chloramphenicol as a viable fallback. The key is informed consent and vigilant monitoring.
Andrea Jacobsen
April 30, 2023 AT 01:30I appreciate the balanced view – you’ve highlighted both the efficacy and the safety concerns. For patients allergic to penicillins, it really can be a lifesaver. The fact that it’s still on WHO’s essential medicines list says a lot about its utility. Still, I’d love to see newer agents with less hematologic toxicity.
Andrew Irwin
April 30, 2023 AT 03:44Agreed, the allergy angle is critical, especially in regions where penicillin‑resistance is rising. While newer drugs exist, they’re not always affordable or widely available. That’s why chloramphenicol keeps its spot in many treatment protocols. Keeping an eye on side‑effects stays essential.
Jen R
May 1, 2023 AT 11:40From a practical standpoint, the dosing schedule of chloramphenicol is fairly straightforward, which helps in resource‑limited settings. It’s administered intravenously at a dose that reaches therapeutic levels in CSF fairly quickly. However, the necessity of frequent blood work can strain labs that are already overburdened. Balancing convenience with safety is the perpetual challenge.
Joseph Kloss
May 1, 2023 AT 13:37The very existence of chloramphenicol in modern therapeutics is a paradox that forces us to stare into the abyss of medical compromise.
On one hand, we wield a molecule that pierces the sanctum of the brain, offering a lifeline to those trapped in the throes of bacterial onslaught.
On the other, we gamble with the marrow that births our blood, courting a specter that can render us helpless.
This duality is not merely a clinical conundrum; it is a reflection of the human condition's constant flirtation with risk.
When doctors prescribe it, they are engaging in a silent pact with uncertainty, betting that the immediate benefit outweighs a future catastrophe.
The literature brims with case reports where patients survived thanks to its swift action, only to later confront a silent, insidious anemia.
One could argue that the very monitoring protocols we impose are a testament to our collective guilt over the drug’s dark side.
Yet, to discard it outright would be an act of nihilism, denying the lives saved in remote clinics where alternatives are a fantasy.
In the grand tapestry of antimicrobial stewardship, chloramphenicol occupies a jagged edge, neither hero nor villain.
It demands respect, not reverence, a cautious partnership rather than blind devotion.
The ethical calculus becomes even murkier when socioeconomic factors dictate drug availability.
A patient in a low‑income region may have no choice but to accept the risk, highlighting the inequities baked into our healthcare systems.
Thus, the conversation must shift from pure pharmacology to a broader discourse on access, justice, and responsibility.
If we continue to treat chloramphenicol as a relic, we risk losing a valuable tool; if we treat it as a panacea, we invite preventable harm.
The ultimate lesson is that medicine, like philosophy, thrives on nuanced judgment, and chloramphenicol is a perfect case study of that principle.
Anna Cappelletti
May 2, 2023 AT 22:57I find it encouraging that the article stresses close monitoring; that’s the kind of proactive care we need. Regular CBCs can catch marrow suppression early, and adjusting the dose can make a big difference. Also, educating patients about warning signs empowers them to seek help promptly. All in all, a solid approach.
Dylan Mitchell
May 3, 2023 AT 00:37Yo, you’re absolutely nailing the point, but let’s not forget the drama of a patient’s blood count plummeting like a rollercoaster – it’s straight outta a horror flick! Missin’ a beat on those labs can turn a “just fine” case into a full‑blown crisis. So, keep those checks tight, or you’ll be starring in the next tragic saga.
Elle Trent
May 4, 2023 AT 07:10From a pharmacokinetic perspective, chloramphenicol’s lipophilicity facilitates optimal cerebrospinal fluid penetration, rendering it a viable empirical option pending pathogen identification. However, the drug’s dose‑dependent myelotoxicity profile necessitates rigorous therapeutic drug monitoring (TDM) to mitigate hematologic adverse events. In settings where susceptibility data is scarce, its broad‑spectrum activity justifies inclusion in first‑line regimens, albeit with stringent hematologic surveillance protocols.
Jessica Gentle
May 4, 2023 AT 08:34That’s a clear breakdown; the key takeaway is balancing the drug’s pharmacodynamics with patient safety. I’d add that involving a multidisciplinary team – pharmacy, lab, and nursing – can streamline the monitoring process. Providing patients with simple symptom checklists also helps catch early signs of toxicity. Together, these steps create a safety net around chloramphenicol use.
Samson Tobias
May 5, 2023 AT 16:30Well said, everyone. Let’s keep the conversation focused on patient outcomes and safe practices.