Most people think back pain is just a muscle strain. But if your pain keeps coming back, especially when you stand or walk, and gets worse over time, it might be something deeper - like spondylolisthesis. This isn’t just a stiff back. It’s when one of your lower spine bones slips forward over the one below it. That slip can pinch nerves, throw off your posture, and make everyday movement painful. And if conservative treatments fail, spinal fusion becomes a real option - but it’s not the only one, and not always the best.
What Exactly Is Spondylolisthesis?
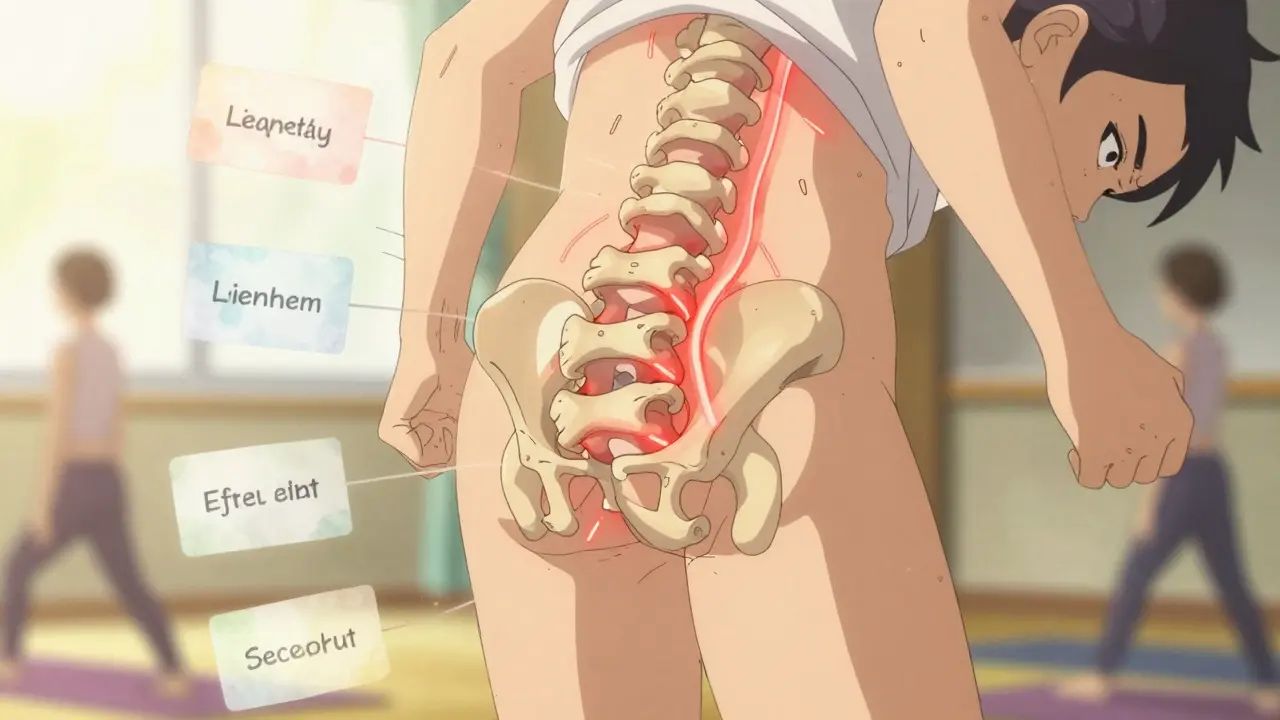
Spondylolisthesis comes from Greek words meaning "vertebra" and "slip." It happens when a vertebra, usually the fifth lumbar bone (L5), slides forward over the sacrum (S1). This isn’t rare. About 6% of adults have it, and it’s more common in women. You might not even know you have it - nearly half of people with the condition never feel pain. But for others, it’s a constant ache in the lower back that radiates to the buttocks and thighs. The pain often feels like a deep muscle strain, but it doesn’t go away with rest like a pulled muscle would. The slippage is measured in grades using the Meyerding scale, from I (less than 25%) to IV (75-100%). Most cases are Grade I or II. But when it hits Grade III or higher, the risk of nerve compression goes up sharply. About 35% of people with severe slips develop tingling, numbness, or weakness in their legs. That’s not just discomfort - that’s nerve damage waiting to happen.Why Does It Happen? Not All Slips Are the Same
Not all spondylolisthesis is created equal. There are five main types, and knowing which one you have changes how you treat it.- Degenerative - This is the most common type in adults over 50. It’s caused by years of wear and tear on the discs and facet joints. Arthritis weakens the structures that hold the spine in place. About 65% of adult cases fall into this category.
- Isthmic - This one starts with a tiny fracture in the pars interarticularis, a small bone bridge connecting vertebrae. It often begins in childhood during sports like gymnastics, football, or weightlifting, where the spine is repeatedly bent backward. The fracture might heal, but the vertebra can slip later in life.
- Dysplastic - A birth defect. The spine just didn’t form right. It’s rare but often shows up in kids under six.
- Pathologic - Caused by diseases like cancer or osteoporosis that weaken the bone.
- Traumatic - From a sudden injury, like a car crash or fall.
What Does It Feel Like? Symptoms Beyond Just Pain
Pain is the big one, but it’s not the only sign. Many people with spondylolisthesis notice:- Tight hamstrings - around 70% of symptomatic patients can’t touch their toes without discomfort.
- Stiffness in the lower back, especially in the morning or after sitting too long.
- Difficulty walking for more than a few minutes without needing to stop and rest.
- A noticeable swayback or, in advanced cases, a rounded upper back (kyphosis).
- Numbness or weakness in one or both legs - a red flag for nerve compression.
How Is It Diagnosed? X-Rays, MRI, and What They Show
You can’t see spondylolisthesis by touch. You need imaging. The first step is always a standing lateral X-ray. That’s key - lying down hides how much the bone actually slips under your body weight. The X-ray shows the grade of slippage and whether there’s a fracture in the pars. If pain radiates down your leg or you have numbness, an MRI is next. It shows if the slipped bone is pressing on nerves or if the discs are worn down. A CT scan gives a clearer picture of the bone structure, especially if surgery is being considered. Here’s something important: the amount of slippage doesn’t always match how much pain you feel. One study found that disc degeneration - not the slip grade - was more closely linked to how long you’ve had symptoms. That means two people with the same slip percentage can feel very different levels of pain. Treatment should focus on symptoms, not just the X-ray.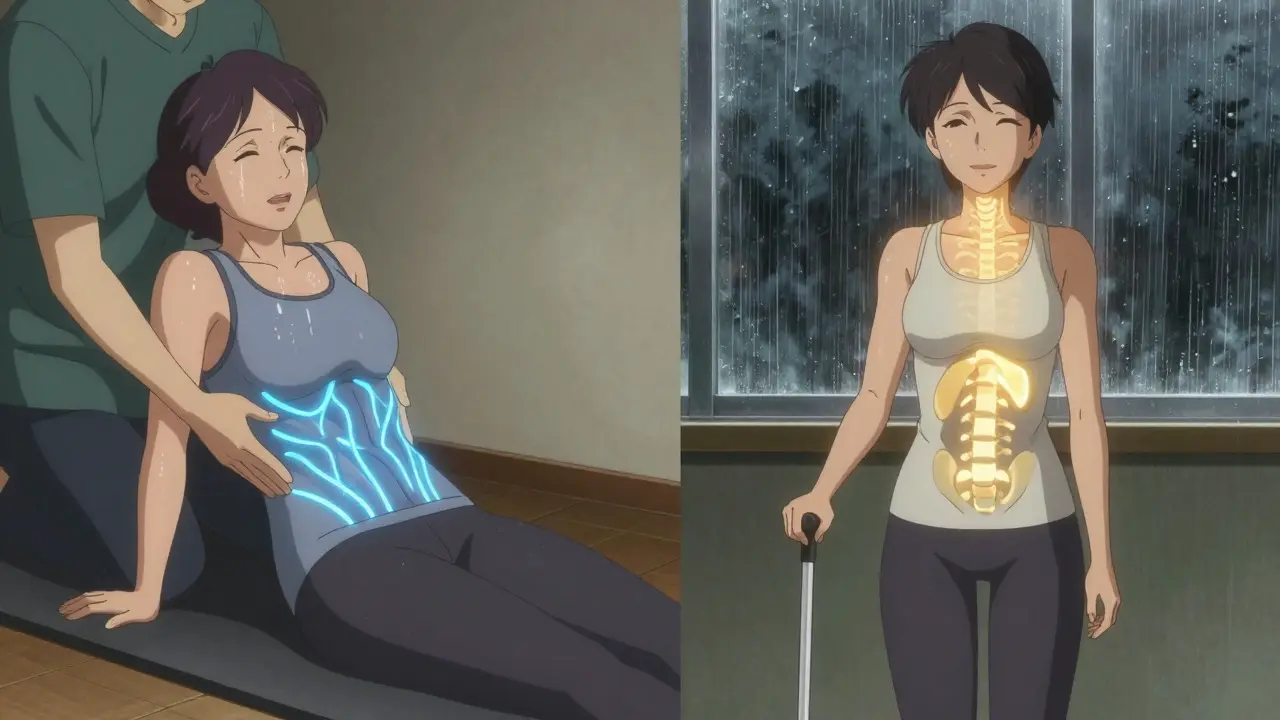
Conservative Treatment: What Actually Works
Most people - 80% or more - never need surgery. The first line is conservative care, and it takes time.- Physical therapy - This isn’t just stretching. It’s core strengthening, pelvic control, and hamstring flexibility. Studies show it takes 12 to 16 weeks of consistent work to see real improvement. Only about 65% of people stick with it long enough.
- Activity modification - Avoid sports or movements that arch your back hard. That means skipping gymnastics, heavy weightlifting, or football if you’re at risk.
- NSAIDs - Ibuprofen or naproxen help with pain and inflammation, but they don’t fix the slip. Use them short-term.
- Epidural steroid injections - If nerve pain is the main issue, these can reduce swelling around the nerve. They’re not a cure, but they can buy time for physical therapy to work.
When Is Fusion Surgery Considered?
Surgery isn’t a first choice. But if you’ve tried 6 to 12 months of conservative care and your pain is still wrecking your life - you can’t sleep, you can’t work, you’re taking painkillers daily - then fusion becomes a real option. There are three main fusion techniques:- Posterolateral fusion - Bone graft is placed along the back of the spine. About 55% of surgeries use this. Success rate: 75-85% for mild slips, but drops to 60-70% for severe ones.
- Interbody fusion (PLIF/TLIF) - The disc is removed and replaced with a spacer, then bone graft is placed between the vertebrae. This restores disc height and opens up nerve space. Used in 35% of cases. Success rate: 85-92% across all grades.
- Minimally invasive fusion - Smaller incisions, less muscle damage. Used in about 10% of cases. Recovery is faster, but long-term results are still being studied.
What Happens After Fusion? Recovery Is a Marathon
Fusion isn’t a quick fix. It’s a long process.- First 6-8 weeks: No lifting, twisting, or bending. You’re in a brace sometimes.
- Months 3-6: Physical therapy focuses on rebuilding strength and movement without stressing the fused area.
- 12-18 months: Full healing. Bone doesn’t fuse overnight.

What Are the Risks? Fusion Isn’t Perfect
Even with a successful fusion, problems can show up later.- Adjacent segment disease - The spine above or below the fusion takes extra stress. About 18-22% of patients develop new pain in those areas within five years.
- Revision surgery - Around 12-15% of people with high-grade slips need another operation later, often because the fusion didn’t hold or adjacent segments broke down.
- Permanent stiffness - You lose some flexibility in the fused area. Most people adapt, but it changes how you move.
What’s New? Alternatives and Advances
Fusion isn’t the only path anymore.- Dynamic stabilization - Devices that limit movement without fusing the spine. They’re promising for Grade I-II slips. Success rates are around 76% at five years - lower than fusion, but no fused segments.
- New fusion devices - FDA-approved in 2022, these spacers are designed to better restore spinal alignment. Early results show 89% fusion rates at six months.
- Bone morphogenetic protein (BMP) - A growth factor that speeds up bone healing. In high-risk patients, it boosted fusion rates to 94% compared to 81% with traditional bone grafts.
- Stem cell therapy - Still experimental, but early trials are looking at using a patient’s own stem cells to help bone grow faster and stronger.
Final Thoughts: It’s Not Just About the Slip
Spondylolisthesis isn’t a death sentence. For many, it’s just a part of aging. For others, it’s a trigger for chronic pain. The key is not to fix the slip - it’s to fix how you feel. If you’re in pain, start with physical therapy. Give it six months. Quit smoking. Lose weight if you need to. Don’t rush to surgery. But if your life is falling apart because of it - if you can’t work, walk, or sleep - then fusion, especially interbody fusion, can give you back your life. The data supports it. The spine doesn’t heal fast. But with the right approach, it can heal right.Can spondylolisthesis heal without surgery?
Yes, in most cases. About 80% of people manage symptoms with physical therapy, activity changes, and pain relief. The bone slip itself rarely reverses, but pain often improves as inflammation decreases and muscles strengthen around the spine. Surgery is only considered if conservative care fails after 6-12 months.
Is walking good for spondylolisthesis?
Walking can be helpful if done carefully. It’s low-impact and helps maintain mobility. But if walking causes leg numbness or forces you to stop frequently, it’s a sign of nerve compression. In those cases, bending forward while walking (like pushing a cart) can reduce pressure on nerves. Avoid long walks on hard surfaces if pain worsens.
Does spondylolisthesis get worse with age?
It can, especially if it’s degenerative. As discs and joints wear down over time, the spine becomes less stable, which can cause the slip to increase. However, not everyone’s condition progresses. Many people stabilize after middle age. Regular core strengthening and weight control can slow or stop progression.
What’s the difference between spondylolysis and spondylolisthesis?
Spondylolysis is a crack or stress fracture in the pars interarticularis - a small bone bridge in the spine. Spondylolisthesis is when that fractured vertebra slips forward. Spondylolysis often comes first, especially in young athletes. Not everyone with spondylolysis develops a slip, but most people with isthmic spondylolisthesis had spondylolysis earlier in life.
How successful is spinal fusion for spondylolisthesis?
Success depends on the type of fusion and the slip grade. Interbody fusion (PLIF/TLIF) has success rates of 85-92% across all grades. Posterolateral fusion works well for mild slips (75-85%) but drops to 60-70% for severe ones. Patient satisfaction is 78-85% at two years. But 12-15% need revision surgery later, often due to adjacent segment issues.
Can you live a normal life after spinal fusion?
Yes, most people return to normal daily activities, including work and light exercise, within a year. High-impact sports like football or heavy lifting are usually discouraged to protect the spine. You’ll lose some flexibility in the fused area, but many adapt well. Long-term, 80% of patients report significant pain relief and improved quality of life.
What happens if spondylolisthesis is left untreated?
If untreated, mild cases may stay stable. But in moderate to severe cases, pain often worsens, nerve damage can progress, and posture may deteriorate - leading to chronic disability. In rare cases, severe slippage can compress the spinal cord or nerves enough to cause loss of bladder or bowel control, which is a medical emergency. Early intervention prevents these outcomes.


Kunal Kaushik
February 3, 2026 AT 14:21Nathan King
February 4, 2026 AT 12:07Antwonette Robinson
February 5, 2026 AT 04:46caroline hernandez
February 6, 2026 AT 13:33Justin Fauth
February 8, 2026 AT 09:12Meenal Khurana
February 9, 2026 AT 18:30Joy Johnston
February 11, 2026 AT 00:23Shelby Price
February 12, 2026 AT 08:15Jesse Naidoo
February 13, 2026 AT 18:01Sherman Lee
February 15, 2026 AT 05:39Lorena Druetta
February 16, 2026 AT 05:39Zachary French
February 16, 2026 AT 10:02Daz Leonheart
February 17, 2026 AT 16:13Amit Jain
February 19, 2026 AT 07:50