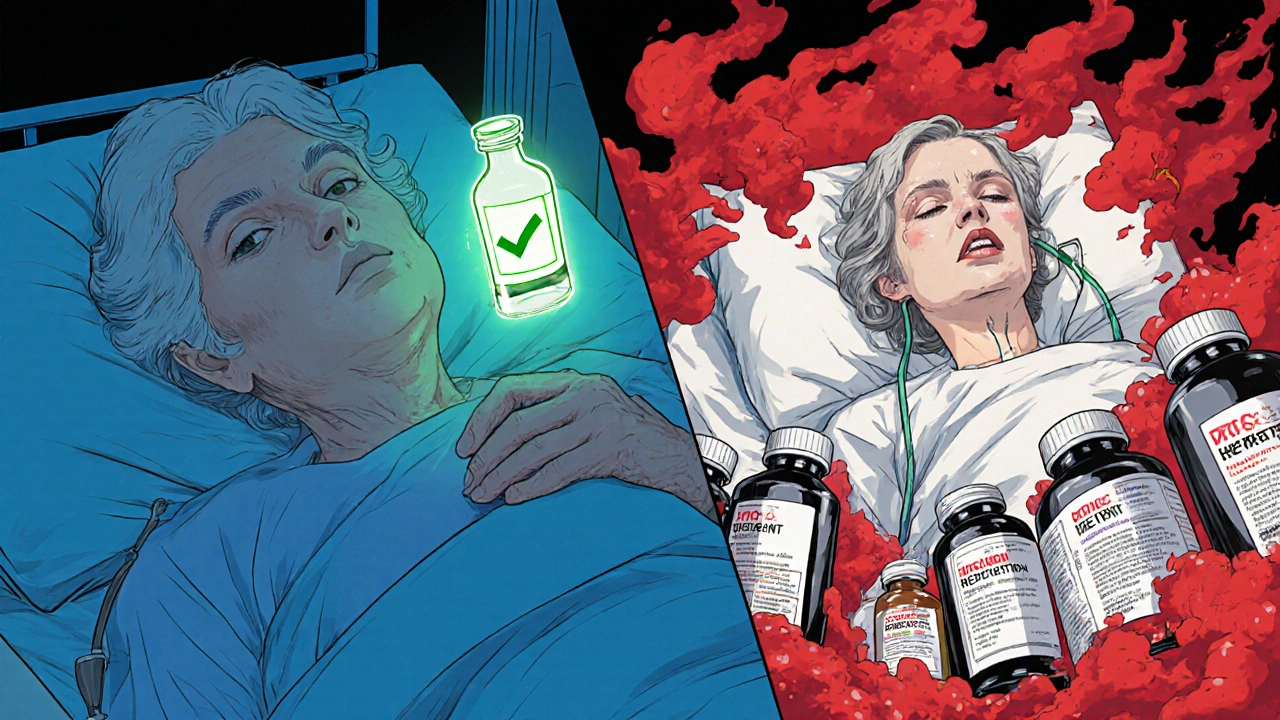
More than 1 in 3 adults over 65 are taking five or more medications every day. That’s not unusual-it’s common. But here’s the hidden danger: many of them are accidentally taking the same active ingredient twice, sometimes three times, without even knowing it. This isn’t a rare mistake. It’s happening every day, in homes across Australia, the U.S., and beyond. And it’s landing people in the hospital.
What Are Double Ingredients?
Double ingredients happen when you take two or more medications that contain the same active chemical. It doesn’t matter if one is a prescription and the other is bought off the shelf. If they both have the same ingredient, you’re doubling your dose. And that can be deadly.The most common example? Acetaminophen. You might be taking a prescription painkiller like Vicodin or Percocet-and also a cold medicine like Tylenol Cold, DayQuil, or a store-brand version. All of them contain acetaminophen. The liver can only handle so much. Too much, and you risk liver failure-sometimes without any warning signs until it’s too late.
The National Institutes of Health reports that over 56,000 emergency room visits each year in the U.S. are caused by unintentional acetaminophen overdose. Most of those cases involve people who didn’t realize they were doubling up.
Other dangerous overlaps include:
- Diphenhydramine (found in Benadryl, NyQuil, ZzzQuil, and some prescription sleep aids) - can cause extreme drowsiness, confusion, and even falls.
- Pseudoephedrine (in Sudafed, Claritin-D, and some cough syrups) - can spike blood pressure and cause heart palpitations.
- NSAIDs like ibuprofen or naproxen (in Advil, Aleve, and some arthritis prescriptions) - can cause stomach bleeding or kidney damage when taken with other NSAIDs or blood thinners.
And here’s the kicker: 45% of prescription labels don’t clearly warn you if the medicine you’re taking shares ingredients with common OTC products. You’re expected to know. But most people don’t.
Why This Happens More Than You Think
It’s not because people are careless. It’s because the system is confusing.Most people see multiple doctors. One for arthritis. One for high blood pressure. One for sleep. Each prescribes something new. No one asks about the cold medicine you took last week. Or the sleep aid you bought online. Or the herbal supplement your sister swore by.
And then there’s the OTC aisle. Aisle 7 at the supermarket is packed with products that all promise relief-but they all hide the same active ingredients behind different brand names. One bottle says “Nighttime Cold & Flu.” Another says “Sleep Aid Maximum Strength.” Both contain diphenhydramine. You take both because you think they’re different.
A 2022 MedlinePlus survey found that 61% of adults have experienced symptoms from double ingredients. The most common? Dizziness, extreme tiredness, and upset stomach. But some end up with internal bleeding, liver damage, or even a trip to the ICU.
One Reddit user, MedSafety101, shared how they took three different cold medicines-all containing pseudoephedrine-thinking they were helping. Within hours, their blood pressure skyrocketed. They ended up in the ER. They didn’t know any of the products had the same ingredient.
Who’s at Highest Risk?
Older adults are the most vulnerable. Why? Because they’re more likely to have multiple chronic conditions-and more medications to manage them.The CDC says adults 65 and older make up 65% of all hospitalizations from double ingredient errors. And it’s not just about age. It’s about complexity.
If you’re taking:
- Five or more prescription drugs
- Three or more OTC medicines
- Any supplements, vitamins, or herbal remedies
- Traditional medicines like Chinese herbs or Ayurvedic pills
-you’re in the danger zone. And if you fill prescriptions at different pharmacies, the risk goes up even more. Pharmacy systems can only flag duplicates if they see all your meds in one place.
A 2021 JAMA Internal Medicine study found that using just one pharmacy reduces double ingredient errors by 63%. Why? Because the pharmacist’s computer can see everything you’re taking-and warn you before you walk out the door.
How to Protect Yourself: 5 Simple Steps
You don’t need a medical degree to avoid this. You just need a list-and the habit of checking it.- Make a full medication list. Write down every single thing you take: prescription, OTC, vitamins, supplements, and herbal remedies. Include the dose and how often you take it. Don’t forget the cough syrup you took last week. Or the magnesium you started for leg cramps. Write it all down.
- Keep it with you. Put a copy in your wallet. Save one on your phone. Give one to a family member. When you go to the doctor or pharmacy, bring it with you. Don’t rely on memory.
- Fill all prescriptions at one pharmacy. It’s the single most effective way to catch duplicates. Pharmacists are trained to spot overlaps. But only if they have the full picture.
- Ask every time you get a new medicine. When a doctor or pharmacist gives you a new pill, say: “Could this have the same ingredient as anything else I’m taking?” Don’t wait for them to ask. Most won’t.
- Review your list every 6 months. Even if nothing changed, things get forgotten. Maybe you stopped taking a pill. Maybe you started a new one. Update your list. Then show it to your doctor.
And here’s a tip: Use the same brand or generic version consistently. Switching between brands can make it harder to track ingredients. If you switch from Tylenol to a store-brand acetaminophen, you might not realize you’re still taking the same thing.
What Doctors and Pharmacies Are Doing About It
The good news? Systems are improving.Since 2022, major electronic health record systems like Epic and Cerner now include automatic “double ingredient checks.” If you’re prescribed a drug that matches something already in your record, the system flags it. But here’s the catch: those systems only see what’s documented. If your OTC meds aren’t in your chart, they won’t catch it.
The FDA started requiring clearer labels on OTC medicines in 2020. Now, every box must show “Active Ingredients” in bold at the top. But a 2023 government report found that 41% of patients still can’t identify duplicates from those labels. People skim. They don’t read.
Pharmacies now offer Medication Therapy Management (MTM) services-free consultations with a pharmacist to review all your meds. In 2022, pharmacists caught double ingredient risks in 87% of these reviews. If you’re on Medicare or have a private plan, ask if you qualify.
The American Geriatrics Society’s Beers Criteria, updated in 2023, now lists 30 high-risk medication combinations-specifically for older adults. Doctors who follow these guidelines are less likely to prescribe dangerous overlaps.
What to Do If You Think You’ve Taken Too Much
If you’ve taken more than one product with the same ingredient and you feel:- Unusually drowsy or confused
- Have nausea, vomiting, or stomach pain
- Feel your heart racing or your blood pressure rising
- Notice yellowing of your skin or eyes
-stop taking everything except your essential meds and call your doctor or go to the nearest emergency room. Don’t wait. Acetaminophen overdose, for example, can cause liver damage without symptoms for 24-48 hours. By then, it’s too late to reverse it.
Bring your medication list. Even if you’re not sure what you took, the list will help them act fast.
Final Thought: This Isn’t Complicated-It’s Just Overlooked
Double ingredient errors aren’t caused by ignorance. They’re caused by a system that assumes you know more than you do. You’re not supposed to memorize chemical names. You’re not supposed to be a pharmacist.You’re supposed to be able to trust that the medicine you’re given won’t hurt you. And with a simple list, a single pharmacy, and three questions asked every time you get a new pill-you can make that true.
Don’t wait for a hospital visit to learn the hard way. Start today. Write down what you take. Keep it with you. Ask the questions. Your body will thank you.
What’s the most common dangerous double ingredient?
The most common and dangerous double ingredient is acetaminophen. It’s found in over 600 prescription and OTC products, including painkillers like Vicodin, cold medicines like Tylenol Cold, and sleep aids like NyQuil. Taking just two of these together can exceed the safe daily limit of 4,000 mg and cause liver damage-even if you don’t feel sick right away.
Can I take two different brands of the same OTC medicine?
No. Even if they have different brand names, they may contain the same active ingredient. For example, Advil and Motrin both contain ibuprofen. Taking both together doubles your dose and increases your risk of stomach bleeding or kidney damage. Always check the “Active Ingredients” section on the label before combining any OTC products.
Do herbal supplements count as medications?
Yes. Herbal supplements like St. John’s Wort, kava, or valerian root can interact with prescription drugs and contain hidden active compounds. They’re not regulated like medicines, so their strength and ingredients vary. Always include them on your medication list-especially if you’re taking blood thinners, antidepressants, or sedatives.
Why don’t doctors always ask about OTC meds?
Doctors often have only 10-15 minutes per visit and focus on the main condition being treated. They assume you’ll mention OTCs-or that they’re harmless. But studies show 67% of patients say their doctors never asked about over-the-counter medicines. That’s why you need to bring your list and say it yourself.
Is it safe to use multiple pharmacies?
It’s riskier. Each pharmacy only sees the prescriptions filled there. If you get a sleep aid from one pharmacy and a painkiller from another, neither system will know they both contain diphenhydramine. Using one pharmacy gives you the best protection-pharmacists can flag overlaps automatically. If you must use multiple pharmacies, always carry your full medication list with you.
Can my phone help me avoid double ingredients?
Yes. Apple Health (iOS 17 and later) now checks for duplicate active ingredients in medications you log. You can manually enter your pills, and the app will warn you if two drugs share the same ingredient. Other apps like MedWise Risk Score also help, but they work best when paired with a printed list and regular reviews with your pharmacist.



Ryan Anderson
November 14, 2025 AT 06:33Just last week I caught myself grabbing both Tylenol and a prescription painkiller without thinking. 😅 Thank you for this post-seriously, I’m printing out the medication list right now. My grandma almost went to the ER last year from the same thing. We’re all guilty of it.
Eleanora Keene
November 15, 2025 AT 17:34This is one of those topics that should be taught in high school. 🙏 I’ve seen so many elderly patients in my clinic who don’t even know what ‘acetaminophen’ means-yet they’re taking three different pills that all have it. Please, everyone: write it down. Keep it simple. Your liver will thank you. And yes, I’m talking to you, Mom.
Joe Goodrow
November 16, 2025 AT 05:39Why is this even a problem? In America we let anyone walk into a pharmacy and buy a bottle of poison labeled as ‘sleep aid.’ In my country, you’d need a license to buy diphenhydramine. This isn’t healthcare-it’s a free-for-all. Stop blaming the patients. Fix the system.
Don Ablett
November 16, 2025 AT 18:20It is noteworthy that the pharmacovigilance infrastructure in North America remains fragmented despite the availability of electronic health records. The absence of centralized medication reconciliation protocols across dispensing entities contributes significantly to iatrogenic harm. One pharmacy adherence alone reduces risk by 63 percent as cited in JAMA. This is empirically robust.
Kevin Wagner
November 18, 2025 AT 02:22Let me tell you something-this isn’t just about pills. It’s about taking back control. You think your doctor’s gonna save you? Nah. You gotta be your own damn superhero. Write the list. Carry it. Ask the question. Slam that pharmacy counter like you own it. And if you’re still taking that ‘natural’ supplement from your cousin’s friend? Burn it. 🔥 Your body didn’t sign up for this circus.
gent wood
November 19, 2025 AT 23:14I’ve been managing polypharmacy for my father for over five years now. He’s 78, on eight prescriptions, three OTCs, and two herbal tinctures. We’ve used MedWise, printed lists, and one pharmacy. It’s made all the difference. No dramatic stories-just quiet, consistent safety. This post is a gift. Thank you.
Dilip Patel
November 20, 2025 AT 10:15USA so dumb why you let old people take 10 pills without training? In India we have Ayurvedic doctor for everything and they know what mix dangerous. You people think medicine is like buying chips from vending machine. LOL. You need to learn from us. Also why you have so many brands for same thing? Stupid.
Jane Johnson
November 22, 2025 AT 00:36Actually, the data on pharmacy consolidation is not universally applicable. Regional variations in prescription tracking systems and insurance interoperability significantly alter outcomes. Additionally, the assumption that patients are incapable of managing their own regimens is patronizing.
Peter Aultman
November 22, 2025 AT 21:58My dad didn’t know Advil and Aleve were the same until he got sick. Now he keeps his list on his fridge with a highlighter. Simple. Dumb? Maybe. But it works. Just check the label. Five seconds. Could save your life.
Sean Hwang
November 23, 2025 AT 07:51Used to work at a pharmacy. Saw this every day. Old lady takes NyQuil and ZzzQuil because one says 'cold' and one says 'sleep'. Same stuff. We’d tell her. She’d say 'but the boxes look different'. Yeah. That’s marketing. Not medicine.
Chris Ashley
November 24, 2025 AT 13:50So what? People die from bad decisions every day. Maybe they shouldn’t be allowed to buy medicine if they’re too dumb to read labels.
kshitij pandey
November 26, 2025 AT 13:02In India, many families share one medicine list printed on paper and kept in the kitchen. Grandparents, parents, kids-all check it before taking anything. Simple. No app needed. Maybe we can learn from each other. This post made me think of my aunt. I’ll send her this right away.