PPI Fracture Risk Calculator
Personalized Risk Assessment
Personalized Assessment
Risk Level:
Estimated Risk Increase:
Recommendations
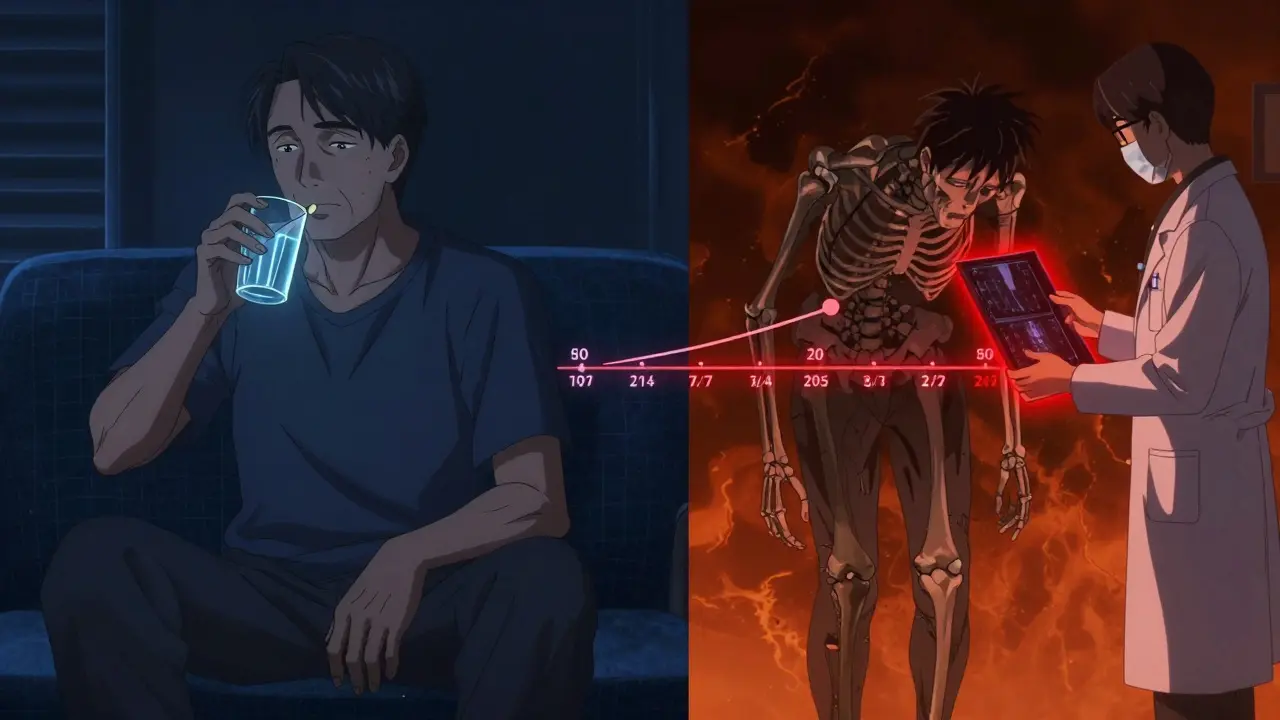
Many people take proton pump inhibitors (PPIs) to manage heartburn, acid reflux, or ulcers. These drugs - like omeprazole, esomeprazole, and lansoprazole - work by shutting down the stomach’s acid production. They’re effective. But over time, especially when used for years, they might be quietly affecting your bones. The link between PPIs and increased fracture risk isn’t theory. It’s backed by data from millions of patients across multiple studies. And if you’re over 65, female, or have other risk factors for osteoporosis, this isn’t something to ignore.
How PPIs Might Weaken Your Bones
Your stomach needs acid to absorb calcium properly. Most calcium supplements - like calcium carbonate - rely on stomach acid to break down and enter your bloodstream. When PPIs lower acid levels too much, your body can’t absorb calcium as well. That doesn’t mean you’ll instantly lose bone density. But over years, if your calcium intake isn’t enough, your bones start to pay the price. Your body pulls calcium from your skeleton to keep your heart, muscles, and nerves working. That leaves your bones weaker.
It’s not just calcium. Some research suggests PPIs might also trigger higher levels of gastrin, a hormone that could interfere with bone remodeling. Other theories point to changes in histamine or magnesium absorption, both of which play roles in bone health. The exact mechanism isn’t fully settled. But the outcome is consistent across studies: long-term PPI use is linked to higher fracture rates, especially in the hip, spine, and wrist.
The Numbers Don’t Lie
Let’s look at real data. A 2019 meta-analysis in the Journal of Bone and Mineral Research reviewed dozens of studies and found that people using PPIs for more than a year had a 20-30% higher risk of hip and spine fractures. The risk climbs with dose and duration. For those taking high doses for seven or more years, the risk of hip fracture nearly quadrupled in one major study. Another study of over 50,000 adults over 50 showed that PPI users had a 27% higher risk of hip fracture compared to those using H2 blockers like famotidine.
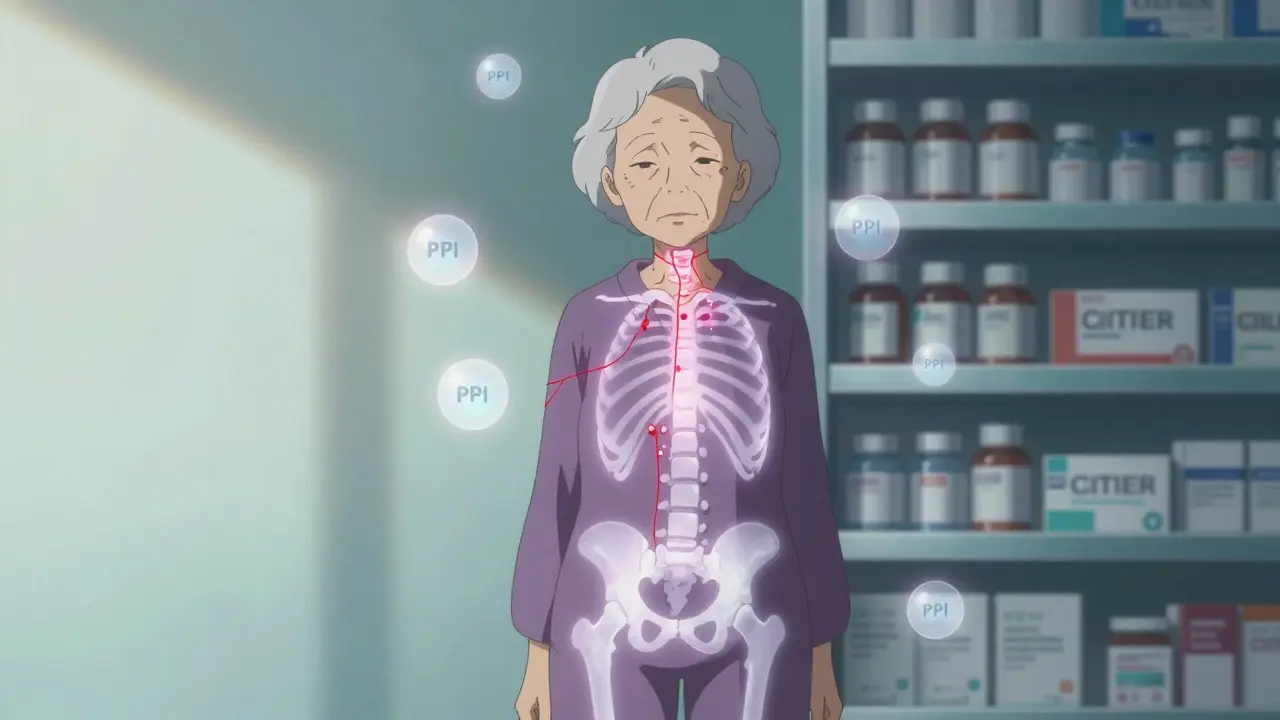
Postmenopausal women are especially vulnerable. One 2019 study found they had a 35% higher risk of hip fracture with long-term PPI use. That’s not because PPIs cause osteoporosis directly. It’s because they add to existing risk factors - lower estrogen, thinner bones, reduced muscle mass. If you’re already at risk, PPIs can tip the balance.
Not All Acid Reducers Are the Same
It’s important to know that not all acid-suppressing drugs carry the same risk. H2 blockers - like ranitidine or famotidine - reduce acid too, but they don’t shut it down as completely as PPIs. Studies comparing the two show that H2 blockers don’t increase fracture risk the same way. One large study of over 110,000 children found no overall fracture risk with H2 blockers, but a small increase in lower-limb fractures with PPIs. In adults, switching from PPIs to H2 blockers may reduce bone-related risk without losing symptom control.
But here’s the catch: PPIs are stronger. For severe GERD, Barrett’s esophagus, or ulcers caused by NSAIDs, they’re often the best tool. The question isn’t whether PPIs are dangerous. It’s whether you really need them - and if you do, how to use them safely.
Who’s Most at Risk?
The fracture risk isn’t equal for everyone. You’re more vulnerable if you:
- Are over 65
- Are a postmenopausal woman
- Have a history of fractures
- Have low body weight (under 57 kg)
- Take corticosteroids like prednisone
- Smoke or drink alcohol regularly
- Don’t get enough calcium or vitamin D
If you fall into one or more of these groups and have been on PPIs for more than a year, it’s time to talk to your doctor. The risk isn’t high for everyone - but for those with multiple risk factors, it’s real enough to warrant action.
What Should You Do If You’re on PPIs?
Don’t stop your medication cold. But do ask these questions:
- Do I still need this drug? Many people stay on PPIs long after their original issue is resolved. A 2017 study found that 60-70% of PPI prescriptions are inappropriate for long-term use. Your doctor can help you test whether you can reduce the dose or stop altogether.
- Am I on the lowest effective dose? Higher doses mean higher risk. If you’re on 40mg of omeprazole daily but only need 20mg, lowering it could cut your fracture risk.
- Could I try intermittent dosing? Instead of daily use, some patients can take PPIs only on days they have symptoms. This reduces total exposure.
- Am I getting enough calcium and vitamin D? If you’re on PPIs, switch to calcium citrate instead of calcium carbonate. Citrate doesn’t need stomach acid to absorb. Aim for 1,200 mg of calcium and 800-1,000 IU of vitamin D daily. Get your blood levels checked if you’re unsure.
- Should I get a bone density test? If you’re over 65, female, and on PPIs for more than 8 weeks, the Endocrine Society recommends a DEXA scan to check your bone density.

What About Alternatives?
If you’re concerned about bone health, there are other options. Lifestyle changes - losing weight, avoiding trigger foods, not eating before bed, elevating the head of your bed - can reduce GERD symptoms without drugs. For mild reflux, antacids or H2 blockers may be enough. If you have ulcers or severe GERD, PPIs are still the gold standard. But you can use them smarter: shorter duration, lower dose, with calcium citrate and vitamin D as backup.
Some patients worry about rebound acid hypersecretion when stopping PPIs. That’s real - but manageable. Work with your doctor to taper slowly, not stop abruptly. Use H2 blockers or antacids temporarily during the transition.
The Bigger Picture
The FDA issued a warning about PPIs and fractures back in 2010. Since then, prescribing patterns have shifted. Between 2015 and 2021, long-term PPI prescriptions among Medicare patients dropped by nearly 20%. That’s progress. But 45% of prescriptions are still inappropriate. That means thousands of people are taking these drugs daily without clear benefit - and quietly increasing their fracture risk.
The American Gastroenterological Association says the absolute risk increase is small. And they’re right. For a healthy 50-year-old with occasional heartburn, the added risk is tiny. But for a 72-year-old woman with osteopenia, a history of falls, and a PPI on her nightstand? That risk isn’t small. It’s urgent.
The goal isn’t to scare you off PPIs. It’s to make sure you’re using them only when needed, at the lowest dose, for the shortest time possible. Your bones will thank you.
Can PPIs cause osteoporosis?
PPIs don’t directly cause osteoporosis, but long-term use can contribute to bone weakening by reducing calcium absorption and possibly interfering with bone remodeling. This increases fracture risk, especially in people already at risk for osteoporosis.
How long do you have to take PPIs before fracture risk increases?
Risk starts to rise after one year of daily use, but it becomes more significant after three to five years. Studies show the highest risk occurs with seven or more years of continuous use, especially at high doses.
Is calcium citrate better than calcium carbonate if I take PPIs?
Yes. Calcium citrate doesn’t require stomach acid for absorption, making it the preferred form for people on PPIs. Calcium carbonate, the cheaper option, needs acid to dissolve - and PPIs reduce that acid, making it less effective.
Should I get a bone density scan if I’m on PPIs?
If you’re over 65, female, and have been on PPIs for more than 8 weeks - especially with other risk factors like low body weight or prior fractures - yes. The Endocrine Society recommends a DEXA scan in this group to assess bone health.
Can I switch from PPIs to H2 blockers to protect my bones?
For mild to moderate acid reflux, H2 blockers like famotidine or ranitidine are a reasonable alternative. They’re less potent than PPIs but don’t carry the same fracture risk. For severe GERD or ulcers, PPIs may still be necessary - but you can reduce dose or frequency to lower risk.
Do I need to take vitamin D with calcium if I’m on PPIs?
Absolutely. Vitamin D helps your body absorb and use calcium. Without enough vitamin D, even calcium citrate won’t help your bones. Aim for 800-1,000 IU daily, and consider a blood test to check your levels if you’re unsure.
Next Steps
If you’re on PPIs long-term, schedule a medication review with your doctor. Bring a list of everything you take - including supplements. Ask: "Is this still necessary?" and "What’s my fracture risk?" Don’t assume you need it just because you’ve been on it for years. Many people can stop or reduce PPIs safely with the right plan.
For those who must stay on PPIs: switch to calcium citrate, get your vitamin D checked, and consider a bone density scan if you’re over 65 or have other risk factors. Small changes can make a big difference in protecting your bones - without giving up the relief you need.


Sazzy De
January 31, 2026 AT 06:59Been on PPIs for 8 years for GERD. Just found out my hip fracture last year might be linked. Feels like a gut punch but also kind of obvious in hindsight.
Switched to calcium citrate and cut my dose in half. Felt better already.
Sheila Garfield
February 1, 2026 AT 03:20My mum’s on PPIs and she’s 71, had a wrist fracture last winter. She never took calcium because she thought it was just for kids. Now she’s on supplements and doing tai chi. Small changes, big difference.
Kimberly Reker
February 1, 2026 AT 05:36Just read this after my doctor told me to get a DEXA scan. I’m 68, female, on omeprazole since 2018. I thought heartburn was just part of aging. Turns out my bones might’ve been paying the price silently.
Going to ask about tapering off and switching to calcium citrate. Thanks for the nudge.
Russ Kelemen
February 2, 2026 AT 01:45It’s funny how we treat symptoms like enemies instead of signals. PPIs silence the fire but don’t ask why the house is burning.
Maybe the real question isn’t whether to stop the drug-but whether we’ve forgotten how to eat, how to sleep, how to live without chemical bandages.
There’s wisdom in reducing, not just replacing.
Shawn Peck
February 3, 2026 AT 13:38Y’all are overthinking this. I’ve been on PPIs since 2010 and I’m still standing. My bones are fine. You’re just scared of big pharma. Stop listening to fearmongers.
Kelly Weinhold
February 4, 2026 AT 05:54Okay but real talk-how many of us are on these because we’re too busy to change our diets? I used to eat pizza at midnight, drink soda, then wonder why I felt like a volcano.
Switched to H2 blockers, started walking after dinner, lost 15 lbs, and haven’t had heartburn in 6 months.
PPIs weren’t the fix. My habits were. And yeah, I took calcium citrate too. Win-win.
KATHRYN JOHNSON
February 4, 2026 AT 23:51As a medical professional, I must emphasize that the data is unequivocal: prolonged PPI use correlates with reduced bone mineral density, particularly in postmenopausal women with low baseline calcium intake. Calcium carbonate is pharmacologically inadequate under acid-suppressed conditions. Calcium citrate is non-negotiable. Vitamin D status must be verified. DEXA screening is indicated after 8 weeks of therapy in high-risk populations per Endocrine Society guidelines. This is not anecdotal-it is evidence-based practice.
kate jones
February 6, 2026 AT 01:41Just want to add something practical: if you’re on PPIs and taking calcium carbonate, you’re wasting your money. I used to take it until my endocrinologist pointed out the pH mismatch. Switched to citrate, got my levels checked, and my T-score improved 0.3 in 9 months.
Also-don’t skip magnesium. It’s often overlooked. PPIs mess with Mg absorption, and low Mg = worse bone turnover. I take 200mg elemental Mg glycinate nightly. No side effects. Big difference.
Sarah Blevins
February 7, 2026 AT 11:29The risk increase is statistically significant but clinically marginal for most. Absolute risk of hip fracture in a healthy 60-year-old on PPIs is less than 0.5% per year. The benefit of controlling GERD often outweighs this. Overzealous deprescribing can lead to esophagitis, Barrett’s, or even adenocarcinoma. Balance matters.
Mike Rose
February 8, 2026 AT 10:36why do people even care about bones anymore? i mean, you gonna be dead one day anyway. just take the pill, eat your pizza, and chill. stop overanalyzing everything.