Why Your Plate Matters More Than You Think
If you’ve been told you have prediabetes, you’re not alone. Nearly 1 in 3 adults in the U.S. has it-and most don’t even know. But here’s the good news: you don’t need medication to turn things around. What you eat every day can cut your risk of developing type 2 diabetes by more than half. It’s not about starving yourself or cutting out carbs entirely. It’s about making smarter choices with fiber, protein, and the type of carbs you eat. And it’s easier than you think.
Fiber: Your Secret Weapon Against Blood Sugar Spikes
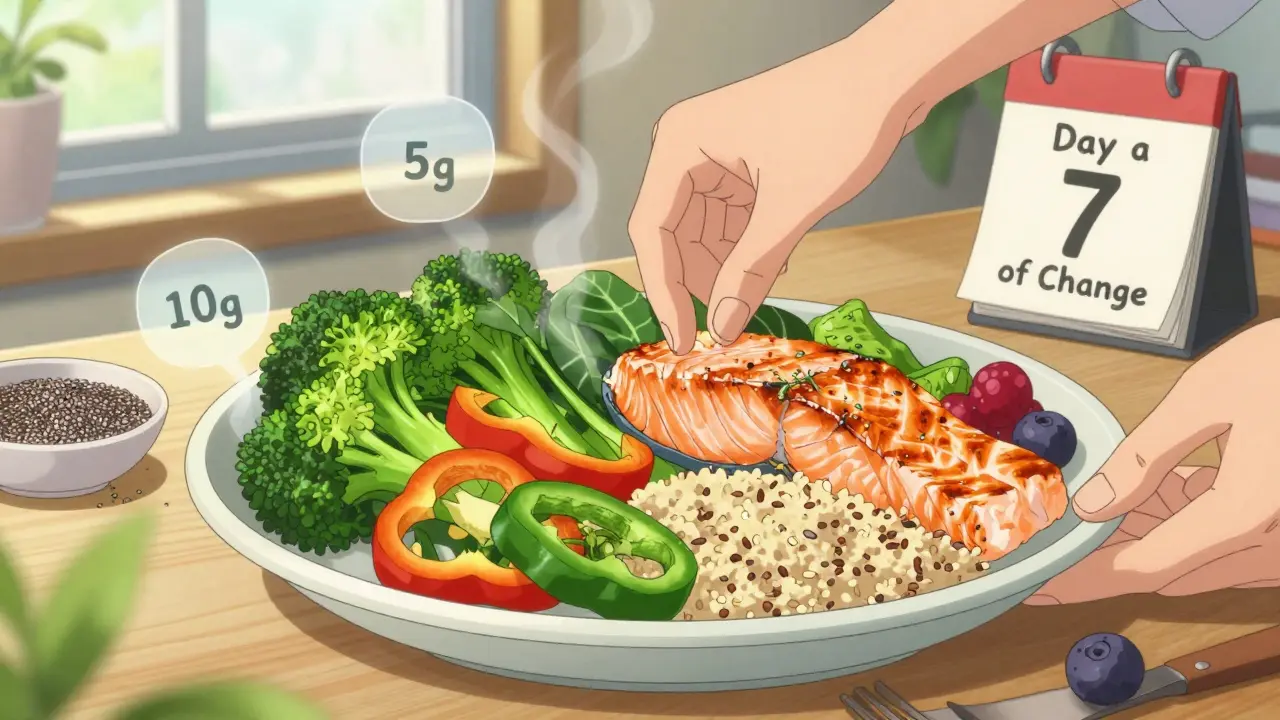
Fiber doesn’t get digested. Instead, it slows down how fast sugar enters your bloodstream. That means your insulin doesn’t have to go into overdrive after every meal. The goal? 25 to 38 grams a day. That’s not as hard as it sounds.
- One cup of broccoli has about 5 grams of fiber.
- A half-cup of lentils? Nearly 8 grams.
- One medium apple with skin? 4.5 grams.
- Two tablespoons of chia seeds? 10 grams.
Most people eat less than half of what they need. Start by filling half your plate with non-starchy vegetables-spinach, peppers, zucchini, cauliflower. They’re low in carbs, high in fiber, and they don’t spike your blood sugar. Swap white rice for barley or quinoa. Choose whole grain bread instead of white. One study found that for every extra 10 grams of fiber you eat daily, your diabetes risk drops by 23%.
Protein: The Silent Stabilizer
Protein doesn’t raise blood sugar much at all. But more than that, it helps your body handle carbs better. When you eat protein with carbs, it slows digestion. That’s why pairing fruit with nuts or yogurt keeps your glucose steady instead of sending it soaring.
Here’s what works:
- 1 cup of berries with 1 ounce of almonds
- 1 small apple with 2 tablespoons of natural peanut butter
- Hard-boiled egg with a slice of whole grain toast
- Grilled chicken or fish with a side of roasted veggies
Lean proteins are key. Chicken, turkey, fish, eggs, tofu, and legumes are all great. Red meat? Limit it. Eating just 100 grams of red meat a day-about the size of a deck of cards-has been linked to a 20% higher risk of diabetes. And processed meats like bacon or sausages? Skip them. They’re loaded with salt and preservatives that make insulin resistance worse.
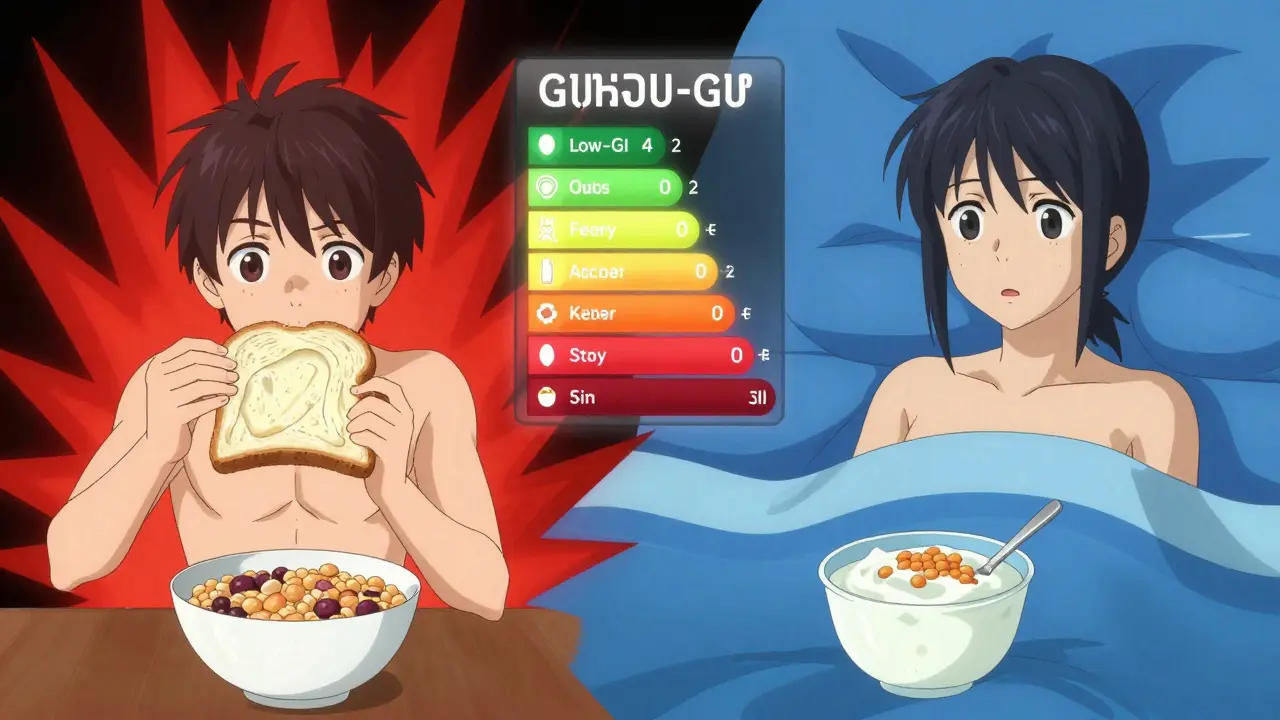
Glycemic Index: Not All Carbs Are Created Equal
The glycemic index (GI) measures how fast a food turns into sugar in your blood. High-GI foods cause quick spikes. Low-GI foods give you steady energy.
Here’s what to avoid:
- White bread (GI 75)
- White rice (GI 73)
- Potatoes (GI 85)
- Sugary cereals
- Soft drinks and fruit juices
And here’s what to choose instead:
- Quinoa (GI 53)
- Sweet potatoes (GI 44)
- Oats (steel-cut or rolled, GI 55)
- Lentils (GI 32)
- Berries (GI 40)
One study showed that after six months on a low-GI diet (average GI of 45), people with prediabetes lowered their HbA1c by 0.5%. That might not sound like much, but it’s enough to move you out of the prediabetes range. The key? Swap one high-GI food at a time. Replace white rice with brown rice. Choose whole grain pasta over regular. Try steel-cut oats instead of instant. Small changes add up.
The Mediterranean Way: It’s Not a Diet, It’s a Pattern
Doctors and dietitians keep pointing to the Mediterranean diet-and for good reason. It’s not about strict rules. It’s about real food: vegetables, fruits, whole grains, beans, nuts, olive oil, fish, and lean protein. It’s low in sugar, low in processed stuff, and high in fiber and healthy fats.
Studies show it improves blood sugar control and reduces heart disease risk, which matters because people with prediabetes are at higher risk for heart problems. You don’t need to eat like someone from Greece. Just focus on:
- More plants
- Less processed food
- Healthy fats (olive oil, avocado, nuts)
- Fish twice a week
- Water or tea instead of soda
It’s flexible. It’s sustainable. And it works.
Portion Control: The Hidden Challenge
Even healthy foods can raise blood sugar if you eat too much. A cup of berries is fine. Three cups? That’s a sugar overload. A small sweet potato is great. A large one with butter? Not so much.
Use the plate method: half your plate = non-starchy veggies. One-quarter = lean protein. One-quarter = whole grains or starchy veggies. That’s it. No counting calories. No measuring cups. Just visual balance.
And don’t forget drinks. Sugary coffee drinks, flavored teas, and fruit juices are sugar bombs. Stick to water, unsweetened tea, or sparkling water with a slice of lemon.
What About Snacks?
Snacks aren’t the enemy. Bad snacks are. If you’re hungry between meals, reach for:
- Handful of raw almonds or walnuts
- Plain Greek yogurt with a few berries
- Carrot sticks with hummus
- A hard-boiled egg
- A small piece of dark chocolate (70% cocoa or higher)
Avoid granola bars, crackers, and fruit snacks. They sound healthy but are often just sugar with a side of fiber.
Real People, Real Results
One person on a diabetes forum switched from instant oatmeal to steel-cut oats and saw their morning blood sugar drop by 30 points. Another started pairing fruit with Greek yogurt and kept their glucose under 140 instead of spiking to 180. These aren’t miracles. They’re simple swaps.
But change is hard. Four out of ten people struggle to eat enough vegetables every day. Portion control is the biggest hurdle for two-thirds of people with prediabetes. That’s why small, consistent steps matter more than perfection.
What to Avoid Completely
Some foods have no place in a prediabetes diet:
- White bread, white rice, pastries
- Sugary cereals and breakfast bars
- Fruit juices and soda
- Processed snacks (chips, cookies, candy)
- Trans fats and hydrogenated oils (found in margarine, fried foods)
- Red and processed meats
It’s not about being perfect. It’s about reducing these as much as possible. If you have a slice of cake at a birthday party? Have it. Then get back to your plan at the next meal.
Progress, Not Perfection
There’s no magic food. No supplement that fixes this. It’s about building habits that last. The Diabetes Prevention Program showed that losing just 5% of your body weight cuts diabetes risk by 58%. That’s 10 pounds for someone who weighs 200. You don’t need to lose 50. Just start moving, eat more fiber, add protein to meals, and choose low-GI carbs.
It’s not about willpower. It’s about structure. Plan your meals. Keep healthy snacks on hand. Cook at home more. Use the plate method. Drink water. Sleep well. Move daily. These aren’t tips. They’re the foundation.
When to Ask for Help
If you’re struggling to make changes on your own, look for a structured program. In Australia, Diabetes Victoria’s ‘Life!’ program has helped over 50,000 people. In the U.S., Medicare covers the National Diabetes Prevention Program. These programs teach you how to eat, move, and manage stress-not just give you a list of dos and don’ts.
You don’t have to do this alone. And you don’t have to wait until it’s too late.
Can I still eat fruit if I have prediabetes?
Yes, absolutely-but choose wisely. Berries, apples, pears, kiwi, and citrus fruits are low in sugar and high in fiber. Stick to one cup at a time. Pair fruit with protein or fat, like a handful of nuts or a spoon of Greek yogurt, to slow sugar absorption. Avoid fruit juices and dried fruit-they’re concentrated sugar without the fiber.
Is the keto diet good for prediabetes?
Some people see quick results on keto, but it’s not the best long-term solution for most. Cutting out entire food groups like whole grains and fruits can make it hard to get enough fiber and nutrients. Plus, it’s tough to stick with. The Mediterranean diet and other balanced, plant-forward plans have more evidence for lasting results. If you’re considering keto, talk to a dietitian first.
How long does it take to reverse prediabetes?
It varies. Some people see improvements in blood sugar within weeks of changing their diet and moving more. But reversing prediabetes usually takes 3 to 6 months of consistent effort. The goal isn’t just to get your numbers back to normal-it’s to keep them there. That’s why building lifelong habits matters more than quick fixes.
Do I need to count carbs?
Not necessarily. Focusing on fiber, protein, and low-GI carbs works better for most people. Use the plate method: half veggies, one-quarter protein, one-quarter whole grains or starchy veggies. That naturally balances your carbs without counting. If you’re using a glucose monitor, you’ll quickly learn which foods spike you-and that’s more useful than any carb count.
Can I drink alcohol with prediabetes?
Moderation is key. Alcohol can cause blood sugar to drop or spike, depending on what you mix it with. Stick to dry wine, light beer, or spirits with soda water and lime. Avoid sugary cocktails, sweet wines, and mixers. Limit yourself to one drink per day for women, two for men. Always eat food when drinking to prevent low blood sugar.
Next Steps: Start Small, Stay Consistent
Here’s your simple starter plan:
- Swap one high-GI food this week (e.g., white bread → whole grain).
- Add one extra serving of vegetables to lunch and dinner.
- Pair your next snack with protein (fruit + nuts, yogurt + berries).
- Drink water instead of soda or juice.
- Walk for 20 minutes after dinner, five days a week.
Do those five things for 30 days. Check your blood sugar if you can. You’ll likely see a difference. And that’s all you need to keep going. You’re not fixing a broken body. You’re giving it the right fuel to heal itself.


Sarah Blevins
January 30, 2026 AT 11:15Melissa Cogswell
January 31, 2026 AT 05:29Blair Kelly
January 31, 2026 AT 16:18Rohit Kumar
February 1, 2026 AT 10:13Lily Steele
February 2, 2026 AT 02:12Beth Beltway
February 2, 2026 AT 23:48Marc Bains
February 3, 2026 AT 07:06Lisa McCluskey
February 3, 2026 AT 15:52owori patrick
February 5, 2026 AT 08:40Mike Rose
February 7, 2026 AT 07:38Russ Kelemen
February 7, 2026 AT 21:01