When your lungs start to feel heavy, your cough won’t quit, and you’re too tired to get out of bed, it’s not just a cold. It could be pneumonia - and not all pneumonia is the same. The type you have changes everything: how you feel, how it’s diagnosed, and most importantly, how it’s treated. Getting the wrong treatment can do more harm than good, especially when antibiotics are used when they shouldn’t be. In the U.S., about bacterial pneumonia is the most common cause, making up half of all cases, while viral and fungal types follow behind with different patterns, risks, and treatments.
Bacterial Pneumonia: The Sudden Onset
Bacterial pneumonia hits fast. One day you might feel fine, the next you’re running a high fever - 102°F to 105°F - with chills, sharp chest pain when you breathe, and a cough that brings up thick, yellow or green mucus. Sometimes, you even see blood in it. Your lips or fingernails might turn blue because your body isn’t getting enough oxygen. This isn’t just a bad cold. It’s your lungs filling up with pus and fluid.
The main culprit? Streptococcus pneumoniae. It’s responsible for over half of all bacterial pneumonia cases in adults and kids. Before vaccines, Haemophilus influenzae type B was a big problem too, especially in children. Now, thanks to routine childhood immunizations, those cases have dropped by more than 90%. But it’s still out there.
Other bacteria like Staphylococcus aureus, Mycoplasma pneumoniae (which causes "walking pneumonia" - milder but lingering), and Legionella pneumophila (linked to contaminated water systems) also cause pneumonia. Legionnaires’ disease, for example, often shows up after staying in hotels or hospitals with dirty air conditioning units.
On an X-ray, bacterial pneumonia looks like a solid white patch - usually on one side of the lung. That’s called lobar consolidation. Doctors hear it too: when they listen with a stethoscope, the affected lung sounds muffled or silent. The body fights back with neutrophils - white blood cells that swarm the infection like firefighters.
Treatment? Antibiotics. Penicillin, amoxicillin, or macrolides like azithromycin work well for most cases. But here’s the catch: if you take antibiotics for something that isn’t bacterial, you’re not helping yourself. You’re just helping bacteria become stronger.
Viral Pneumonia: The Slow Burn
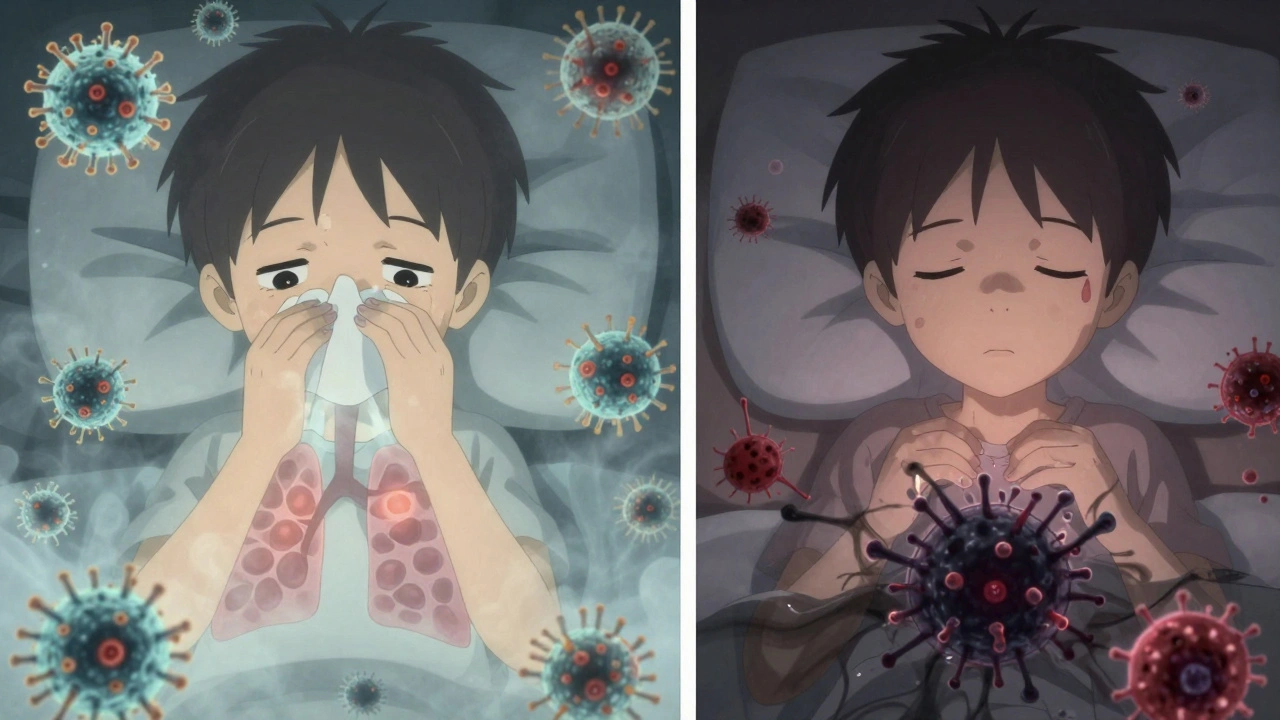
Viral pneumonia doesn’t come crashing in. It creeps up. You start with a runny nose, sore throat, maybe a low-grade fever. Then, over three to five days, it moves deeper. Your cough gets worse - dry at first, then maybe producing clear or white mucus. You feel achy, exhausted, and your chest feels tight. Unlike bacterial pneumonia, your fever usually stays under 102°F.
The usual suspects? Influenza A and B, RSV (respiratory syncytial virus), rhinovirus (the common cold virus), and SARS-CoV-2 (the virus that causes COVID-19). During flu season, about 20-30% of pneumonia cases are viral. In kids under five, RSV is the leading cause.
On an X-ray, viral pneumonia doesn’t show one solid white patch. Instead, it looks like a foggy haze across both lungs - called interstitial infiltrates. That’s because the virus attacks the walls between the air sacs, not the sacs themselves. Your immune system floods the area with lymphocytes, causing swelling and mucus buildup everywhere.
There’s no magic pill for most viral pneumonia. Rest, fluids, and fever reducers are the mainstays. But for influenza, antivirals like oseltamivir (Tamiflu) can help if taken within 48 hours of symptoms. For severe COVID-19 pneumonia, remdesivir may be used in hospitals.
Here’s the dangerous twist: viral pneumonia often opens the door for a secondary bacterial infection. About 25-30% of people with severe flu develop bacterial pneumonia on top of it - usually from Streptococcus pneumoniae or Staphylococcus aureus. That’s why doctors watch closely after a viral illness. If symptoms suddenly worsen after a few days, it might be a bacterial takeover.
Fungal Pneumonia: The Hidden Threat
Fungal pneumonia is rare in healthy people. But if you have a weak immune system - from HIV, chemotherapy, organ transplants, or long-term steroid use - it becomes a serious risk. You won’t catch it from someone else. You breathe it in from the environment.
The big three in the U.S.? Coccidioides (Valley fever), Histoplasma, and Blastomyces. These fungi live in soil - especially in the Southwest (Coccidioides), the Ohio and Mississippi River valleys (Histoplasma), and the Southeast (Blastomyces). Farmers, construction workers, gardeners, and cave explorers are at higher risk. If you’re digging in dirt or cleaning up bird droppings, you’re stirring up spores.
Symptoms? Fever, cough, chest pain, fatigue - sounds like the others, right? But fungal pneumonia can also cause joint pain, rashes, or even spread to the skin or brain. It mimics bacterial or viral pneumonia so well that many cases are misdiagnosed at first.
Diagnosis requires special tests: sputum cultures, blood tests, or even a lung biopsy. A regular chest X-ray might show patchy shadows, but it won’t tell you it’s fungal. You need specific lab work.
Treatment? Antifungals. Not antibiotics. Medications like fluconazole, itraconazole, or amphotericin B are used, depending on the fungus and how sick you are. Treatment can last months. For people with weakened immune systems, lifelong suppression might be needed.
There’s no vaccine for fungal pneumonia. Prevention means avoiding dusty environments if you’re immunocompromised. Wearing a mask during yard work or construction can help. In high-risk areas, doctors sometimes recommend it.
How to Tell Them Apart
It’s not always easy - symptoms overlap a lot. But here’s a quick guide:
- Onset: Bacterial = sudden. Viral = gradual. Fungal = slow and sneaky.
- Fever: Bacterial = high (102-105°F). Viral = mild to moderate (100-102°F). Fungal = variable, often low-grade.
- Cough: Bacterial = thick, colored mucus. Viral = dry or clear mucus. Fungal = may be bloody or contain debris.
- X-ray: Bacterial = one solid white area. Viral = foggy, both lungs. Fungal = patchy, irregular shadows.
- Who’s at risk? Bacterial = everyone. Viral = kids, elderly, flu season. Fungal = immunocompromised, outdoor workers.
Doctors now use rapid PCR tests that check for 20+ viruses and bacteria from one nasal swab. These tests are getting faster and more accurate - some give results in under two hours. That means less guessing and better treatment faster.
Prevention: What Actually Works
You can’t avoid all pneumonia, but you can slash your risk.
For bacterial pneumonia: Get the pneumococcal vaccine. There are two types: PCV20 (Prevnar 20) and PPSV23. Adults 65+ should get both, spaced a year apart. Kids get a series starting at 2 months. These vaccines cut pneumonia risk by 60-70%.
For viral pneumonia: Get your flu shot every year. It reduces pneumonia risk by 40-60%. Stay up to date on your COVID-19 boosters - they cut pneumonia risk by 90% in the first few months after vaccination.
For fungal pneumonia: Avoid soil and dust if you’re immunocompromised. Wear an N95 mask when gardening, cleaning chicken coops, or working in dusty construction sites. If you live in an endemic area and have a weakened immune system, talk to your doctor about preventive antifungals.
Smoking increases your risk by 2.3 times. Quitting is one of the best things you can do for your lungs - no matter your age.

Why Getting It Right Matters
Every year in the U.S., pneumonia sends about 1 million people to the hospital and kills 50,000. Bacterial pneumonia has the highest death rate among hospitalized patients - 5-7%. Fungal pneumonia kills up to 15% in people with weak immune systems. Viral pneumonia kills 3-5%, but flu-related pneumonia can hit 9% in seniors.
And here’s the silent crisis: about 30% of antibiotic prescriptions for pneumonia are unnecessary. That’s because doctors can’t always tell right away if it’s bacterial or viral. Each unnecessary antibiotic helps create superbugs - bacteria that no drug can kill. That’s not just your problem. It’s everyone’s.
That’s why rapid testing, better vaccines, and smarter prescribing are the future. Researchers are now looking at blood biomarkers - tiny signals in your blood - that can tell if an infection is bacterial or viral within minutes. If it works, we could cut inappropriate antibiotic use by 40%.
Pneumonia isn’t one disease. It’s three - each with its own rules, risks, and remedies. Knowing the difference doesn’t just help you feel better. It saves lives - yours and others’.
Can you have pneumonia without a fever?
Yes, especially in older adults, young children, or people with weakened immune systems. In these groups, pneumonia may present with confusion, dizziness, extreme fatigue, or a drop in body temperature instead of a high fever. Don’t wait for a fever to seek help - if you’re struggling to breathe or feel worse than usual, get checked.
Is viral pneumonia contagious?
Yes. Viral pneumonia itself isn’t directly contagious, but the viruses that cause it - like flu, RSV, and COVID-19 - are. You spread them through coughs, sneezes, or touching surfaces. That’s why handwashing, masks, and staying home when sick are critical. You might give someone a cold that turns into pneumonia, especially in high-risk people.
Can fungal pneumonia be cured?
Yes, but it takes time. Antifungal medications like fluconazole or itraconazole can clear the infection, but treatment often lasts months - sometimes years - especially for people with HIV or who’ve had organ transplants. Stopping treatment too early can lead to relapse. Regular follow-ups and blood tests are essential.
Do I need a chest X-ray if I think I have pneumonia?
Not always, but it’s the best way to confirm it. Doctors often diagnose pneumonia based on symptoms and listening to your lungs. But if you’re not improving, are over 65, have other health problems, or are very sick, an X-ray is standard. It shows the location and type of infection, which guides treatment.
Can you get pneumonia twice?
Yes. Having pneumonia once doesn’t make you immune. You can get it again from a different virus, bacterium, or fungus. That’s why vaccines and prevention are so important - especially if you’re at higher risk due to age, smoking, or chronic illness.
What to Do Next
If you’ve had a lingering cough, fever, or trouble breathing for more than a few days - see a doctor. Don’t wait. Don’t self-diagnose. Don’t take leftover antibiotics. Tell your doctor about your symptoms, any recent travel, exposure to birds or soil, or if you’re on immune-suppressing meds.
If you’re over 65, smoke, have diabetes, COPD, or heart disease, ask your doctor about pneumococcal and flu vaccines. If you work outdoors or live in a high-risk area, talk about fungal exposure risks. Prevention isn’t just smart - it’s lifesaving.
Pneumonia doesn’t care if you’re young or old. But knowledge does. Know the signs. Know your risks. Know the difference - and act before it’s too late.



Audrey Crothers
December 12, 2025 AT 06:02Just had pneumonia last winter-viral, turned bacterial after 5 days. Docs gave me amoxicillin and I was back on my feet in 10 days. 🙌 Don’t wait if you’re fading. Get checked. Seriously.
Laura Weemering
December 13, 2025 AT 18:48Interesting how we’ve reduced bacterial pneumonia via vaccines… but now we’re creating a new crisis: antifungal resistance. We’re just swapping one apocalypse for another, aren’t we? The system is a house of cards-built on profit, not prevention. And don’t get me started on Big Pharma’s role in delaying rapid diagnostics…
Stacy Foster
December 13, 2025 AT 19:57Wait… so you’re telling me the government doesn’t want us to know that fungal pneumonia is caused by 5G towers? I live near a cell tower and got sick after gardening. Coincidence? Or is this another CDC cover-up? I’ve seen the documents. They’re hiding the truth. They don’t want you to know you can get it from WiFi routers. I’m not paranoid-I’m prepared.
Reshma Sinha
December 14, 2025 AT 20:34As a respiratory therapist in Mumbai, I see this every monsoon-fungals in soil, kids with RSV, elders with bacterial pneumonia. Vaccines save lives. Period. No debate. Get the shots. Wear masks. Stay dry. Simple. Not complicated. Just do it.
Robert Webb
December 16, 2025 AT 11:32I appreciate how thorough this breakdown is. One thing I’d add: the difference in immune response between bacterial and viral pneumonia isn’t just about white blood cells-it’s about cytokine profiles. Bacterial triggers a massive neutrophil surge, while viral tends to activate interferons and T-cells. That’s why rapid biomarker tests are so promising-they’re not just detecting pathogens, they’re reading the body’s alarm system. We’re moving toward precision medicine, and that’s huge.
nikki yamashita
December 17, 2025 AT 19:24My grandma had pneumonia and didn’t have a fever-just kept falling asleep in her chair. We thought she was tired. Turns out, she was dying. Don’t ignore fatigue. It’s not laziness. It’s your body screaming.
wendy b
December 19, 2025 AT 14:24Actually, the stats on fungal pneumonia are wildly overstated. Most cases are misdiagnosed as TB or even lung cancer. The CDC’s data is outdated-based on 2008 surveillance. And amphotericin B? That’s a toxic relic. We’ve got newer azoles now, but insurance won’t cover them unless you’re in a tertiary center. This is a class issue, not a medical one.
Rob Purvis
December 19, 2025 AT 18:55Just wanted to say-thank you for mentioning Legionella. I worked in a hotel cleaning AC units for years. We never wore masks. I got sick twice. No one told us. This is occupational hazard. We need better safety standards for janitorial staff. Not just for pneumonia-also for mold, asbestos, all of it. It’s not just a health issue-it’s a labor rights issue.
Lawrence Armstrong
December 20, 2025 AT 20:59Got my flu shot last October. Still got sick. But I didn’t end up in the hospital. Vaccines aren’t perfect, but they’re the best tool we’ve got. I’m not anti-vax-I’m pro-survival. 🤝
Donna Anderson
December 21, 2025 AT 23:26my mom got fungal pneumonia after cleaning out her attic-she thought it was just allergies. took 6 months to get better. now she wears a mask to garden. smart lady. you guys should too. dont be dumb.
Levi Cooper
December 23, 2025 AT 05:40Why do we even have this problem? In my country, people just take antibiotics and get better. Why is America so weak? You have all the tech, all the money, and still you die from pneumonia? It’s because you don’t take responsibility. Stop blaming doctors. Take care of yourselves. Quit smoking. Stop eating junk. Simple.
sandeep sanigarapu
December 25, 2025 AT 01:25As someone from rural India, I’ve seen children with pneumonia treated with leftover antibiotics from older siblings. No tests. No X-rays. Just hope. This article is a lifeline for places like mine. Please share it with clinics, schools, community centers. Knowledge is the only vaccine we can’t patent.
Ashley Skipp
December 26, 2025 AT 08:19So viral pneumonia is contagious but not pneumonia itself? That’s a semantic trick. You’re just playing with words. If the virus spreads and turns into pneumonia then the pneumonia is contagious. Stop overcomplicating things.
Nathan Fatal
December 27, 2025 AT 23:50What’s really being avoided here is the philosophical question: if pneumonia is a symptom of systemic failure-of healthcare access, of environmental neglect, of antibiotic overuse-then treating it as a medical event rather than a societal one is a form of denial. We diagnose lungs, but we ignore the world that poisoned them. The real cure isn’t in a pill-it’s in justice.
Adam Everitt
December 29, 2025 AT 05:52Actually, I think the author underestimates the role of air pollution in predisposing people to pneumonia-especially in urban areas. PM2.5 particles damage cilia, make mucus thicker, and weaken defenses. It’s not just germs-it’s the air we breathe. And we’re all breathing the same poisoned sky. The real epidemic isn’t pneumonia-it’s the failure to clean our atmosphere.