Penicillin Allergy Assessment Tool
Assess Your Reaction
This tool helps you determine if your past reaction to penicillin was likely a true allergy or a side effect. Based on CDC guidelines and medical research.
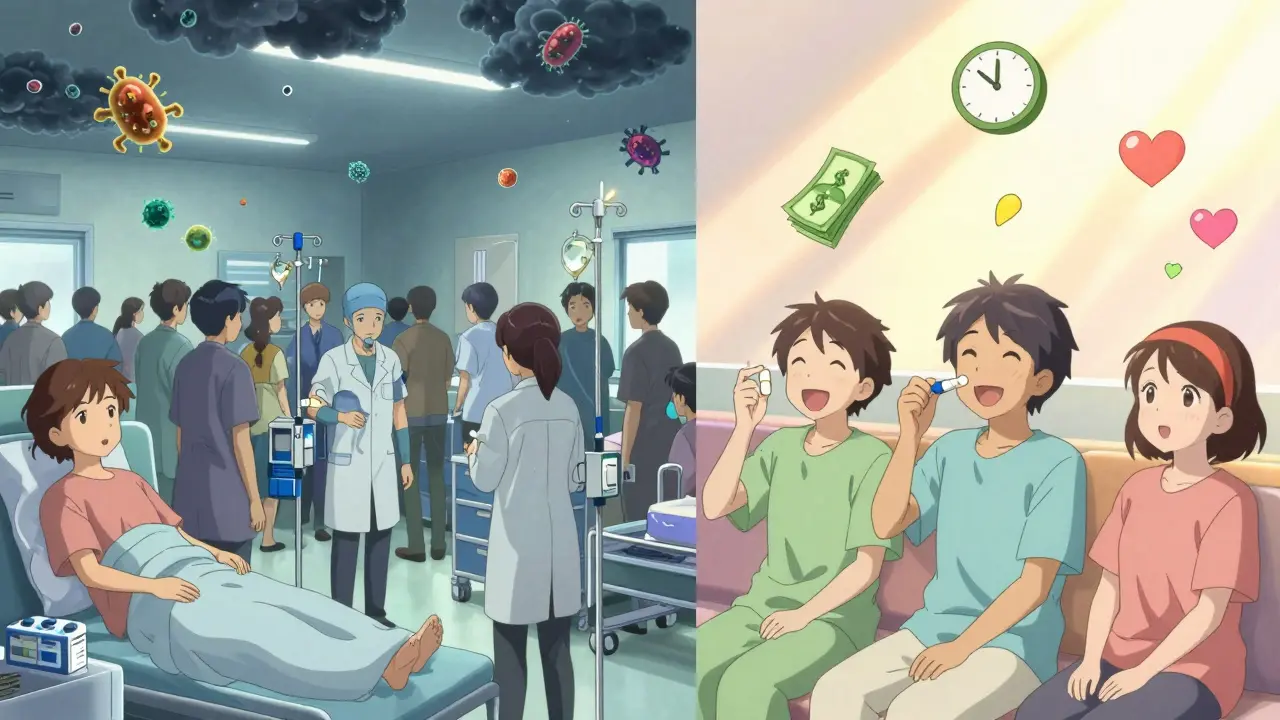
More than 10% of people in the U.S. say they’re allergic to penicillin. But here’s the shocking part: over 90% of them aren’t. If you’ve been told you’re allergic to penicillin because you got a rash as a kid, had nausea after taking it, or your mom said you were allergic - you might be carrying around a label that’s not just wrong, but dangerous.
What’s the real difference between an allergy and a side effect?
It’s simple: an allergy is your immune system reacting like it’s under attack. A side effect is your body just not handling the drug well. Mixing them up is common - and costly.
If you have a true penicillin allergy, your body makes IgE antibodies that trigger a rapid, potentially life-threatening response. Think hives, swelling of the lips or throat, trouble breathing, or a sudden drop in blood pressure. These usually show up within minutes to an hour after taking the drug. This is what doctors call an immediate-type reaction. It’s rare - affecting less than 1% of people who think they’re allergic - but it’s serious.
On the other hand, side effects are common, predictable, and harmless in most cases. Nausea? That’s a side effect. Diarrhea? Side effect. A mild, itchy rash that shows up days later? Also usually a side effect. These don’t involve your immune system at all. They’re just how your stomach, gut, or skin reacts to the medicine.
Here’s the problem: doctors often don’t ask enough questions. A child gets a rash while sick with mono - the rash is from the virus, not the penicillin. But the label sticks: “Allergic to penicillin.” Ten years later, that person gets pneumonia. Instead of a simple, cheap penicillin, they get a stronger, more expensive antibiotic. And that’s where the real danger starts.
Why mislabeling penicillin allergies is a public health crisis
When people are wrongly labeled allergic to penicillin, they get different antibiotics. Not just any alternatives - usually broader-spectrum drugs like vancomycin, clindamycin, or fluoroquinolones. These are stronger, more expensive, and far more likely to cause other problems.
Take Clostridioides difficile (C. diff), a nasty gut infection that causes severe diarrhea and can be fatal. People given broad-spectrum antibiotics are 2.5 times more likely to get it than those who get penicillin. In fact, the CDC found that C. diff rates jump from 5.5 to 12.5 cases per 1,000 patient-days when penicillin is avoided unnecessarily.
And it’s not just infection risk. Patients with mislabeled allergies have a 6-in-1,000 higher chance of dying within a year after hospitalization. Why? Because they’re treated with less effective drugs, stay in the hospital longer, and face more complications.
The financial toll is huge too. A 2018 study in JAMA Internal Medicine found that each hospital stay for someone with a mislabeled penicillin allergy costs about $1,000 more. Multiply that by millions of patients, and you’re looking at over $20 billion in extra healthcare costs every year in the U.S. alone.

Most penicillin reactions aren’t allergies - here’s how to tell
Let’s break down what’s actually happening when people think they’re allergic:
- Upset stomach, nausea, vomiting - Very common. Happens in 5-10% of users. Not an allergy. Just your gut being sensitive.
- Mild rash (maculopapular) - Appears days after starting the drug. Often happens with viral infections like mononucleosis or Epstein-Barr. This is a drug rash, not an allergy. In fact, over 80% of these rashes are not immune-related.
- Diarrhea - Affects 1-2% of people. Usually mild and goes away. Caused by gut bacteria disruption, not an immune response.
- Vaginal yeast infection - Common in women. Antibiotics kill good bacteria, letting yeast overgrow. Totally normal side effect.
- Headache, dizziness - Non-specific. Could be from the illness, dehydration, or the drug. Not an allergy.
True allergic reactions look different. They come fast. They involve swelling, trouble breathing, hives, or low blood pressure. If you’ve ever had to use an EpiPen or been rushed to the ER after taking penicillin - then yes, you likely have a real allergy. But if your reaction was a rash, a stomach ache, or a fever that went away on its own? You probably don’t.
How to find out if you’re truly allergic - and why you should
There’s a simple, safe, three-step process to confirm or rule out a penicillin allergy:
- Talk to your doctor - Be specific. When did it happen? How long after taking the drug? What exactly happened? Did you need epinephrine? Or just an antihistamine? The more detail you give, the better.
- Get skin tested - A specialist (allergist or immunologist) will use tiny amounts of penicillin derivatives on your skin. If you’re truly allergic, you’ll get a raised bump. It’s quick, safe, and accurate. Skin testing catches over 95% of true allergies.
- Take a small dose under supervision - If the skin test is negative, you’ll be given a small oral dose of amoxicillin (a penicillin-type drug) and watched for an hour. This is the gold standard. In studies, over 99% of people who pass this step tolerate penicillin perfectly.
And here’s the kicker: if you had a reaction more than 10 years ago, there’s an 80% chance you’re no longer allergic. Your immune system forgets. Studies show IgE antibodies fade over time. You don’t need to avoid penicillin forever just because you had a rash as a child.
Real stories - and why testing changes lives
One woman from Ohio spent 25 years avoiding penicillin after a childhood rash. She got pneumonia twice. Each time, she was given vancomycin - a powerful IV drug with kidney risks. Her hospital stays were longer. Her bills were higher. After testing, she found out she wasn’t allergic. Now she takes penicillin without fear. Her next infection? Treated in three days. Cost? Half as much.
A 2021 survey of 1,200 people who got tested found that 78% were scared to do it. But 99.2% had zero reaction during the test. Afterward, 67% said their antibiotic costs dropped. 58% had shorter hospital stays. 42% finally cleared up chronic infections they’d been struggling with for years.
And the barriers? Mostly fear and lack of access. Many primary care doctors don’t know how to refer patients. Insurance doesn’t always cover testing. But things are changing. Hospitals in the U.S. are now running pharmacist-led allergy de-labeling clinics. One program in Kaiser Permanente tested 15-20 patients a week and successfully removed the allergy label from 92% of them.
What’s next? Testing could become routine
By 2025, hospitals will be financially rewarded for reducing unnecessary antibiotic use. That means they’ll push hard to fix mislabeled allergies. The CDC has even released a smartphone app - the Penicillin Allergy Assessment Tool - that helps doctors decide who needs testing based on simple answers.
And in the next five years, experts predict that asking about penicillin allergies will be as routine as checking your blood pressure. Electronic health records now include prompts to review allergy labels. If you’ve been told you’re allergic, your doctor may soon ask: “When was that? What happened? Have you ever been tested?”
Don’t wait. If you’ve ever been told you’re allergic to penicillin - even if it was decades ago - talk to your doctor. Ask about testing. It’s safe. It’s fast. And it could save you money, time, and maybe even your life.



Gloria Ricky
February 12, 2026 AT 04:10Jason Pascoe
February 12, 2026 AT 13:32Sonja Stoces
February 13, 2026 AT 14:43Annie Joyce
February 14, 2026 AT 14:03Luke Trouten
February 15, 2026 AT 18:44Kristin Jarecki
February 17, 2026 AT 09:58Jonathan Noe
February 18, 2026 AT 19:11Suzette Smith
February 20, 2026 AT 16:52Jason Pascoe
February 22, 2026 AT 15:05