Have you noticed your nails turning yellow, thickening, or separating from the skin underneath? You’re not alone. About fungal nail infection and nail psoriasis affect millions of people every year-and most of them get them mixed up. The symptoms look almost identical: discolored nails, crumbling edges, and that unsettling gap between the nail and nail bed. But here’s the thing-treating one like the other doesn’t just waste time. It can make things worse.
What’s Actually Going On With Your Nails?
Fungal nail infections, or onychomycosis, are caused by tiny organisms like Trichophyton rubrum that sneak in through small cuts or damp environments. These fungi feed on keratin-the same protein your hair and nails are made of. Over time, they turn the nail yellow, brown, or even black. The infection usually starts at the tip or side of the nail and creeps inward. You might also notice a foul smell, which is a dead giveaway. Nail thickening is common too, often reaching 3 to 5 millimeters thick-so thick you can’t trim it without clippers. Nail psoriasis, on the other hand, isn’t caused by germs. It’s your own immune system going haywire. Instead of skin cells taking 28 to 30 days to renew, they rush to the surface every 3 to 4 days. This overload builds up under and around the nail, causing damage. You won’t smell anything, but you’ll see tiny pits like pinpricks on the surface. Or maybe you’ll spot salmon-colored patches under the nail-translucent, reddish-yellow blotches that look like oil stains. These are called oil-drop lesions. The nail might lift away from the bed, or you’ll get chalky white buildup underneath.The Big Differences You Can’t Ignore
At first glance, both conditions look like nail problems. But if you know what to look for, the clues are clear.- Nail pitting: Small dents in the nail surface? That’s psoriasis. Found in 70% of cases. Almost never seen in fungal infections.
- Foul odor: If your nail smells bad, it’s almost certainly fungal. Psoriasis doesn’t cause odor.
- Where it starts: Fungal infections begin at the tip or side of the nail and grow slowly. Psoriasis often hits multiple nails at once, sometimes suddenly.
- Thickening: Fungal nails get really thick-3 to 5 mm. Psoriatic nails thicken too, but usually only to 2 to 3 mm.
- Other symptoms: If you have scaly skin on your elbows, knees, or scalp, and now your nails are acting up? That’s a red flag for psoriasis. About 95% of nail psoriasis cases happen in people who already have skin psoriasis.
One study found that 78% of psoriasis patients had nail pitting, while only 2% of fungal cases did. That’s not a coincidence. And here’s another key point: psoriasis doesn’t spread from person to person. Fungal infections do. You can pick them up from gym floors, public showers, or even sharing nail clippers.
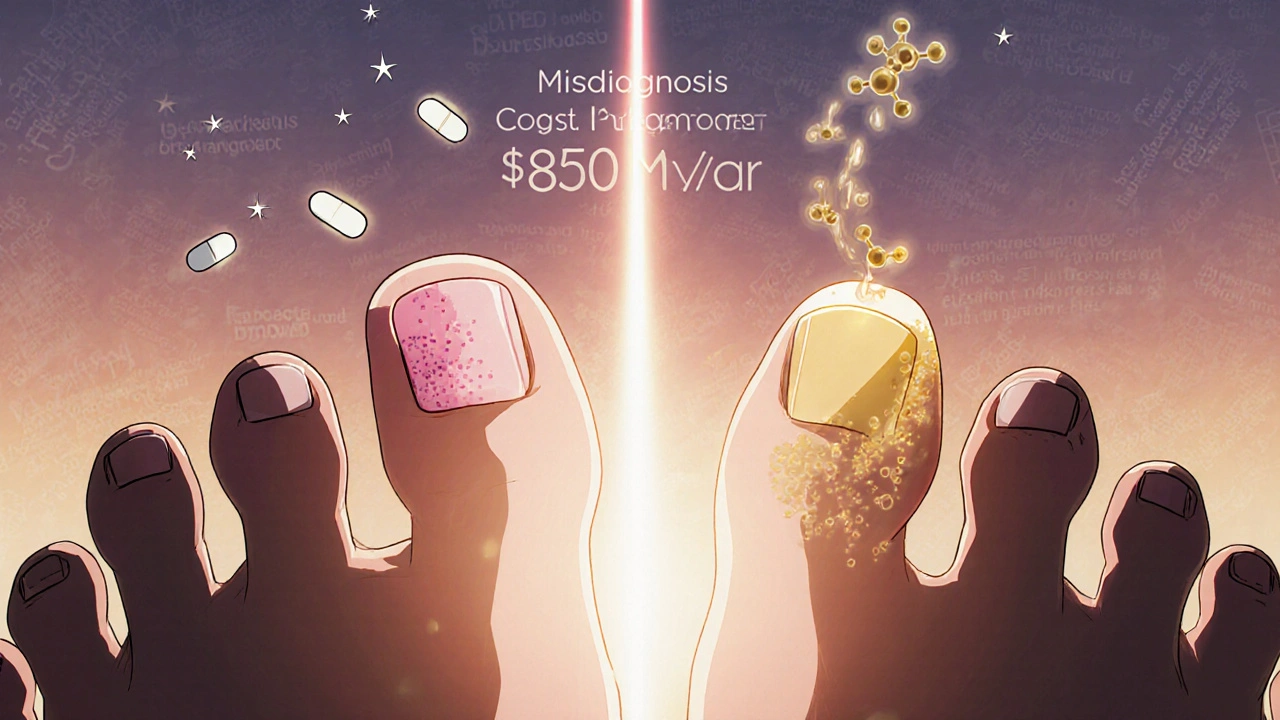
Why Misdiagnosis Is So Common-and So Costly
Doctors get it wrong about 30 to 40% of the time. Why? Because most nail changes look similar to the untrained eye. A yellow, thickened nail? Easy to assume it’s fungal. But if it’s actually psoriasis, antifungal creams won’t help. They’ll just delay real treatment. A 2023 survey of 2,850 patients found that 78% of people with nail psoriasis waited six months or longer before getting the right diagnosis. Some tried antifungals for over a year. Their nails got worse. One person on a patient forum wrote: “After 8 months of antifungal treatments that did nothing, my nail separated completely. It hurt to wear shoes.” The reverse happens too. People with fungal infections get told it’s psoriasis and given steroid creams or injections. Those can dry out the nail even more, making it brittle and prone to breaking. One user on a foot health forum said: “They told me it was psoriasis and gave me steroid shots. My nail started crumbling like paper.” Misdiagnosis isn’t just frustrating-it’s expensive. In the U.S. alone, unnecessary treatments for these conditions cost about $850 million a year. That’s billions globally.
How Doctors Actually Diagnose This
You can’t rely on sight alone. Even dermatologists need help. Here’s the real diagnostic process:- Clinical exam: The doctor looks for pitting, oil spots, or salmon patches. If they’re there, it’s likely psoriasis.
- KOH test: A tiny scraping of the nail is mixed with potassium hydroxide and looked at under a microscope. This finds fungal elements in 70-80% of cases. Quick, cheap, and usually done in the office.
- Fungal culture: If KOH is negative but suspicion remains, a sample is sent to a lab. It takes weeks to grow, but it’s 95% specific. If fungus grows, you’ve got an infection.
- PAS staining: This is a more sensitive lab test that highlights fungal threads in tissue. It’s used when KOH and culture are unclear.
For psoriasis, doctors might use the Nail Psoriasis Severity Index (NAPSI), which scores damage across four parts of the nail. It’s not perfect, but it helps track progress over time.
Advanced tools like reflectance confocal microscopy are now being used in research clinics. In a 2023 Mayo Clinic study, this imaging technique correctly identified the condition in 92% of cases-far better than visual exams alone. But it’s still mostly in academic centers, not your local dermatologist’s office.
Treatment: What Actually Works
Fungal infections need antifungals. Oral meds like terbinafine work best. Most people see clearance after 12 weeks. Topical treatments like efinaconazole (Jublia) are less effective but avoid liver side effects. The catch? Toenails grow slowly-only 0.1mm per day. So even if the fungus dies, it takes 9 to 12 months for a healthy nail to grow out completely. You have to be patient. Nail psoriasis responds to different tools. Topical steroids applied under the nail can help. Injections of corticosteroids directly into the nail bed show results in 8 to 12 weeks. For moderate to severe cases, biologics like secukinumab (Cosentyx) or ixekizumab are game-changers. A 2022 survey found 65% of patients saw major improvement after 24 weeks on these drugs. These aren’t quick fixes-they’re long-term immune system modulators.And here’s something most people don’t know: psoriasis nails are more likely to get a secondary fungal infection. About 4.6% to 30% of psoriasis patients develop both. That’s why testing for fungus is critical-even if you already have psoriasis.
What You Can Do at Home
For fungal infections:- Keep feet dry. Use antifungal powder daily.
- Avoid walking barefoot in public showers or pools.
- Change socks twice a day if you sweat a lot.
- Don’t share nail clippers or files.
For psoriasis:
- Moisturize nails and cuticles daily with thick creams or ointments.
- Avoid trauma. Don’t bite your nails or pick at the cuticles.
- Use gentle nail tools-no aggressive filing.
- Photograph your nails monthly under the same lighting. It helps you and your doctor track changes.
Don’t try home remedies like vinegar soaks or tea tree oil for fungal infections. They’re not backed by solid evidence. And never use steroid creams on suspected fungal nails-they can make the fungus spread.
What’s Coming Next
Research is moving fast. Scientists are now studying the microbiome of the nail bed. Early findings show psoriasis nails have more Staphylococcus bacteria and less Cutibacterium, while fungal nails are loaded with Trichophyton DNA. This could lead to simple swab tests that tell you exactly what you’re dealing with. AI tools are being trained to analyze nail photos. One project predicts a 22% drop in misdiagnosis by 2027. Climate change is also a factor-warmer, wetter conditions are expanding where fungi can live. Experts expect fungal infections to rise by 15% over the next decade.When to See a Doctor
If your nails have changed in the last few months, especially if:- They’re thick, discolored, or separating
- You have skin psoriasis or eczema
- You’ve tried antifungals for months with no improvement
- You’re in pain or the nail is crumbling
Don’t wait. See a dermatologist. General practitioners miss these diagnoses half the time. Dermatologists get it right 85% of the time. That’s the difference between months of frustration and months of healing.
Can fungal nail infections go away on their own?
No. Fungal nail infections don’t clear up without treatment. The fungus lives deep in the nail bed and keeps growing. Left untreated, it can spread to other nails or even the skin around the nail. In people with diabetes or poor circulation, it can lead to serious infections. Treatment is necessary to remove it.
Is nail psoriasis contagious?
No. Nail psoriasis is an autoimmune condition, not an infection. You can’t catch it from someone else. It’s caused by your immune system attacking your own nail tissue. However, if you have psoriasis, you’re more likely to get a secondary fungal infection-which *is* contagious.
Why do my nails keep getting worse even after using antifungal cream?
If you’re using antifungal cream and your nails are still thickening, lifting, or changing color, you might not have a fungal infection. Nail psoriasis looks very similar but won’t respond to antifungals. The cream may even dry out your nails and make them more brittle. Get a KOH test or see a dermatologist to confirm the diagnosis.
How long does it take to treat nail psoriasis?
It varies. Topical treatments like steroid injections can show improvement in 8 to 12 weeks. Biologic drugs like secukinumab take about 24 weeks for full results. Because nails grow slowly, it can take 6 to 12 months for a completely healthy nail to replace the damaged one-even after the inflammation is under control.
Can I use over-the-counter nail polish to hide the discoloration?
It’s not recommended. Regular nail polish traps moisture, which can worsen fungal infections. Even if you have psoriasis, polish can irritate the nail bed and make separation worse. If you want to cover it, use a breathable, antifungal nail polish like those containing ciclopirox-but only after confirming your diagnosis. Better yet, let your nails breathe while you treat the root cause.



linda wood
December 1, 2025 AT 12:50So let me get this straight-I spent $200 on antifungal cream for 8 months because my nails looked like they’d been through a wood chipper, and it turns out my immune system was just being dramatic? Thanks, body. I’m now convinced my nails are just passive-aggressive little drama queens.
Also, who the hell thought ‘oil-drop lesions’ was a good name for something that looks like a grease stain on a napkin? Someone in dermatology has a dark sense of humor.
Anyway, I finally saw a derm after my big toe started smelling like a gym sock left in a locker for a decade. KOH test came back clean. Psoriasis. I cried. Then I bought a new pair of shoes. And a therapist.
TL;DR: Stop guessing. Get tested. Your feet will thank you.
Also, if you’re using vinegar soaks, please stop. You’re not pickling your toenails for a salad.
Joy Aniekwe
December 3, 2025 AT 03:13How is it possible that in the 21st century, with all our genomic sequencing and AI diagnostics, we still rely on a drop of nail clipping and a microscope to tell if your nail is infected or if your immune system is having a tantrum? We can map Mars but can’t tell the difference between a fungus and a faulty immune response without a 19th-century lab technique.
And yet, millions suffer while doctors shrug and say, ‘Try this cream.’
It’s not incompetence-it’s systemic neglect. Nail health is ‘cosmetic.’ So we treat it like a fashion choice, not a biomarker.
Meanwhile, in Nigeria, women with psoriatic nails are told it’s ‘spiritual’ and given herbal baths that do nothing. The global medical hierarchy is a joke.
At least here, you can get a KOH test. In some places, you get a prayer and a pamphlet.
Richard Thomas
December 3, 2025 AT 19:17It is, in fact, a matter of considerable scientific and clinical import that the differential diagnosis between onychomycosis and nail psoriasis remains a persistent diagnostic challenge, despite the considerable advances in dermatopathological methodology over the past three decades. The clinical overlap, as elucidated in the seminal work of Korman et al. (2021), is not merely superficial but rooted in shared histopathological manifestations of keratinocyte dysregulation, albeit with divergent etiological pathways.
Furthermore, the economic burden attributable to misdiagnosis, as cited in the U.S. healthcare expenditure literature, exceeds $850 million annually-an amount that, if reallocated toward standardized diagnostic protocols, could significantly reduce the prevalence of iatrogenic exacerbation. The current reliance on KOH microscopy, while cost-effective, exhibits a sensitivity of only 70–80%, which is statistically insufficient for definitive clinical decision-making.
It is therefore imperative that primary care providers be mandated to refer all cases of suspected nail dystrophy to dermatologists with access to PAS staining and, where available, reflectance confocal microscopy. The absence of such protocols constitutes a systemic failure in preventive dermatology.
One might also posit that the rise in fungal prevalence is correlated with the increasing global incidence of urbanization and the concomitant increase in exposure to shared, poorly ventilated, moisture-retentive environments. Climate change, as referenced in the text, is not a peripheral consideration but a central etiological factor in the epidemiological shift.
It is regrettable that laypersons continue to self-diagnose using anecdotal forums, thereby perpetuating therapeutic inertia and delaying definitive intervention. The nail is not a canvas for cosmetic concealment-it is a window into systemic physiology.
Sara Shumaker
December 5, 2025 AT 05:55I’ve been living with psoriasis for 15 years, and I never realized my nails were part of it until my daughter pointed out the pitting. She’s 12. She noticed it before my dermatologist did.
It made me think-how many of us are just living with this, thinking it’s normal? Like, yeah, my nails are weird, but that’s just how they are. We normalize pain. We normalize isolation. We normalize being told ‘it’s just your nails.’
But your nails aren’t ‘just your nails.’ They’re part of your body’s story. And if your body is trying to tell you something, maybe we should stop ignoring it because it’s not ‘visible’ enough.
Also, if you’re reading this and you’ve been told your nail problem is ‘fungal’ and nothing worked? You’re not crazy. You’re not lazy. You just needed someone who knew how to listen.
Let’s stop making people feel like their symptoms are too weird to be real. They’re not weird. They’re just underdiagnosed.
Steven Howell
December 6, 2025 AT 23:52As someone who has spent over a decade traveling across Southeast Asia and working in rural clinics, I can confirm that the misdiagnosis of nail conditions is not a first-world problem-it is a global one. In rural Thailand, I saw a woman with severe onychomycosis being treated with herbal poultices for two years. In Cambodia, a man with psoriatic nails was given antifungal pills because the local clinic had no access to KOH testing.
The tools we take for granted-microscopes, cultures, dermatoscopes-are luxuries in many parts of the world. Yet the symptoms are universal.
What’s needed isn’t just better diagnostics, but better education for frontline health workers. A simple flowchart-‘Pitting? Oil spots? Smell? Multiple nails?’-could save thousands of patients from years of ineffective treatment.
And yes, biologics are amazing. But if you can’t even get a $5 KOH test, you’ll never get to the biologics.
Let’s not forget that medicine is not just about innovation-it’s about accessibility.
Robert Bashaw
December 8, 2025 AT 16:04My nails used to look like they’d been through a horror movie. Yellow. Crumbly. Smelled like a dead raccoon in a gym sock. I tried everything-tea tree oil, vinegar baths, garlic paste (yes, really), even a ‘nail detox’ from a TikTok influencer who claimed it was ‘toxic mold’.
Turns out? My immune system was throwing a tantrum like a toddler who didn’t get ice cream. Psoriasis. No fungus. Just my body deciding my nails were the enemy.
Now I get steroid shots. They hurt like hell. But my nails? They’re growing back like tiny pink soldiers. I’m not crying. I’m not. (I am.)
Also, if you’re using nail polish to hide it? Stop. You’re basically putting a Band-Aid on a gunshot wound. Let your nails breathe, you beautiful, broken, glorious creatures. They’re trying to heal.
And if you’ve been told it’s fungus for years? I feel you. We’re all just trying to grow out of our own skin. Literally.
Brandy Johnson
December 9, 2025 AT 00:36Let’s be honest-this whole ‘nail psoriasis vs. fungus’ debate is just another example of how the medical establishment has been manipulated by pharmaceutical lobbying. Who benefits from misdiagnosis? Companies selling $500 biologics and $200 antifungal creams. Not patients.
And why are we even talking about ‘KOH tests’? Why not just ban all over-the-counter antifungals and force every patient to get a proper lab diagnosis first? Because bureaucracy. Because profit.
Meanwhile, Americans waste billions on treatments that don’t work while people in developing countries die from infections they can’t even name.
It’s not a medical issue. It’s a moral failure dressed in white coats.
And if you think this is ‘just about nails’-you’re missing the point. It’s about who gets care, who gets ignored, and who gets billed.
Peter Axelberg
December 10, 2025 AT 10:23My dad had fungal nails. He was a mechanic. Worked with his hands. Never wore shoes in the garage. Got it from the oil-soaked floor. Tried everything. Finally got terbinafine. Took a year for the nail to grow out. He said it was the most patient he’d ever been in his life.
My sister? Psoriasis. No smell. Just pits. Took her three years to get diagnosed because every doctor assumed it was fungus. She’s on biologics now. Her nails look like normal nails again. She says it’s the first time in 15 years she’s worn sandals.
Point is: your nails don’t lie. But people? They’re bad listeners.
Don’t be the person who ignores the signs. Don’t be the one who says ‘it’s probably nothing.’ It’s never nothing.
And yeah, I know it’s just nails. But sometimes, the little things are the ones that keep you from living.
Get checked. Seriously. Your future self will thank you.