When someone is diagnosed with multiple sclerosis (MS), the real fear isn’t just the relapses-it’s what happens between them. The slow, quiet decline that no one talks about. You might feel fine for months, even years, after a flare-up. But inside your brain and spinal cord, something deeper is breaking down. And most treatments today don’t stop it.
What Really Goes Wrong in Multiple Sclerosis
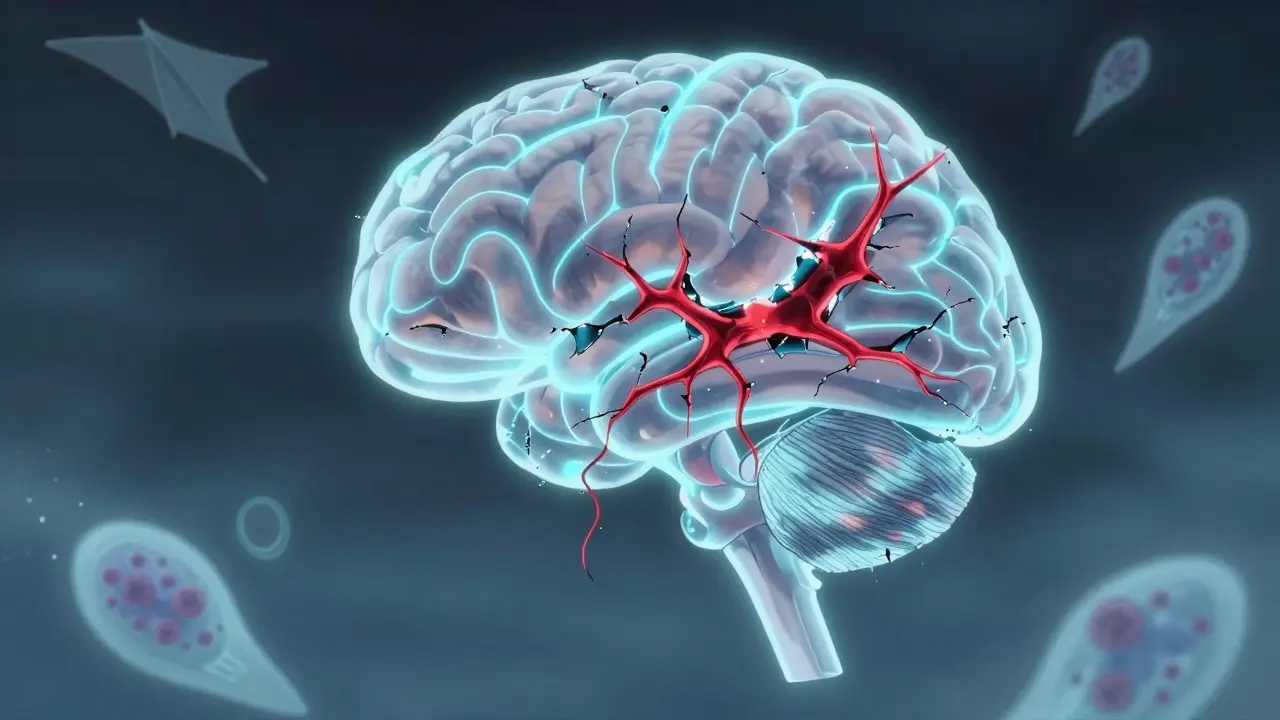
Multiple sclerosis isn’t just about inflammation. That’s the part we see on MRI scans-the bright spots, the flare-ups, the sudden numbness or blurred vision. But those are just the symptoms of a much bigger problem. At its core, MS is an autoimmune disease where the body’s own immune system attacks the myelin sheath-the fatty insulation that wraps around nerve fibers in the brain and spinal cord. Without myelin, electrical signals slow down or get blocked. That’s why you might stumble, lose sensation, or struggle to focus.
But here’s the key point most people miss: myelin can repair itself. The body has cells called oligodendrocytes that can regrow this insulation. That’s why many people recover after a relapse. The real damage doesn’t come from the inflammation alone. It comes from what happens to the nerve fibers underneath.
When myelin is stripped away repeatedly, the axon-the actual nerve fiber-starts to degenerate. Think of it like a power cable with its insulation worn off. The wire doesn’t just stop working. Over time, it begins to fray, shrink, and eventually die. This isn’t reversible. Once an axon is gone, the connection between your brain and your body is permanently broken.
Studies show that up to 40% of people with relapsing-remitting MS (RRMS) will eventually shift into a phase called secondary progressive MS (SPMS). In this stage, symptoms keep getting worse, even when there are no new flare-ups. No new lesions on MRI. No fever. No obvious trigger. Just a steady decline. Why? Because the damage is no longer about inflammation-it’s about the slow, silent death of nerve cells.
The Hidden Drivers of Progression
For years, doctors thought MS was mostly driven by immune cells attacking from outside the central nervous system. But newer research shows that once the disease moves into its progressive phase, the fight shifts inside the brain itself. B cells-immune cells that usually make antibodies-start gathering in the meninges, the protective layers around the brain. These cells form structures that look like lymph nodes. And they’re not just sitting there. They’re pumping out chemicals that slowly poison the surrounding tissue.
One study found that people with these B-cell clusters in their brains had MS symptoms start about 10 years earlier than those without them. They also had higher disability scores and a 2.3 times greater risk of dying sooner. This isn’t just correlation-it’s a warning sign that the disease has changed its game.
And it’s not just B cells. Microglia, the brain’s own immune cells, become overactive. They don’t clean up debris-they start chewing on healthy nerve fibers. At the same time, mitochondria-the energy factories inside nerve cells-start failing. Without enough energy, axons can’t maintain their structure. Sodium channels, which help nerve signals jump from one point to another, disappear. The nerve fibers literally starve to death.
What makes this worse is that the brain tries to compensate. fMRI scans show other parts of the brain lighting up to take over lost functions. But this is like using a backup generator to power a whole city. It works for a while. Eventually, the system burns out. That’s why disability keeps climbing even when inflammation fades.

Why Current Treatments Fall Short
There are 21 FDA-approved disease-modifying therapies (DMTs) for MS. Most of them-interferons, glatiramer acetate, fingolimod, ocrelizumab, natalizumab-work by suppressing the immune system. They reduce relapses by 30% to 50%. For someone in the early stages of RRMS, that’s life-changing. Fewer hospital visits. Less time off work. Better quality of life.
But here’s the problem: none of them stop axonal degeneration. They don’t protect nerves. They don’t rebuild myelin. They don’t fix mitochondrial failure. They just turn down the volume on inflammation. That’s why, after 10 to 15 years, many patients still end up in SPMS. The drugs bought them time-but not a cure.
And in progressive MS? These drugs barely work. Ocrelizumab, one of the few approved for primary progressive MS, only slows disability progression by about 25% over three years. That’s not a reversal. It’s a delay. And even that benefit fades over time.
That’s why doctors now say: if you’re still having relapses after two years on a DMT, you’re not responding well. It’s not just about reducing lesions. It’s about preventing long-term damage. The goal isn’t just to stop flare-ups-it’s to keep your nerves alive.
What’s Coming Next: The New Frontiers
The next wave of MS treatments isn’t about immunosuppression. It’s about neuroprotection. Researchers are now testing drugs that target the real killers: energy failure, sodium overload, and failed repair.
One promising area is sodium channel blockers. When axons lose myelin, they flood with sodium. That overloads their energy systems. A drug called ranolazine, originally used for heart conditions, is now being tested in MS. Early trials show it may reduce nerve damage and improve walking speed.
Another approach targets mitochondria. Drugs like idebenone and riboflavin help nerve cells produce more energy. In a 2023 trial, patients with SPMS who took idebenone for 48 weeks showed less brain atrophy and better cognitive scores than those on placebo.
And then there’s remyelination. Scientists are testing compounds that wake up the brain’s own repair cells. One drug, opicapone, which blocks an enzyme that inhibits myelin growth, showed signs of myelin repair in early MRI scans. Another, bexarotene, a cancer drug repurposed for MS, triggered oligodendrocyte regeneration in animal models.
There are currently 17 active Phase II and III trials focused on progressive MS. For the first time, researchers aren’t just asking: “Can we stop inflammation?” They’re asking: “Can we save the nerve?”

What You Can Do Now
While these new drugs are still in testing, there are things you can do today to slow damage:
- Get your vitamin D levels checked. Low vitamin D is linked to higher relapse rates and faster progression. Aim for 40-60 ng/mL. Many people need 5,000 IU daily.
- Quit smoking. Smokers with MS progress 3 times faster than non-smokers. The chemicals in tobacco directly damage nerve cells.
- Exercise regularly. Aerobic activity increases brain-derived neurotrophic factor (BDNF), a protein that supports nerve survival. Walking, swimming, or cycling 30 minutes a day, 5 days a week, can improve mobility and slow decline.
- Monitor brain atrophy. Standard MRI shows lesions, but it misses the real story. Ask your neurologist about whole-brain volume measurements. Gray matter loss is a stronger predictor of disability than new lesions.
- Track your function, not just your score. The Expanded Disability Status Scale (EDSS) is outdated. The Multiple Sclerosis Functional Composite (MSFC) measures walking, hand movement, and thinking. Ask for this test every 6 months.
The Big Picture
MS is no longer just an inflammatory disease. It’s a neurodegenerative one. And the clock is ticking from the moment you’re diagnosed. The inflammation you see today is the axonal damage you’ll feel in 10 years. That’s why early, aggressive treatment matters-not just to stop relapses, but to protect what’s underneath.
The old model of MS treatment was: treat the flare, wait for the next one. The new model is: protect the nerve, every day. We don’t have all the answers yet. But we know enough to act differently. The goal isn’t just to live with MS. It’s to live well-with your nerves intact.
Can you reverse nerve damage in multiple sclerosis?
No, once an axon is lost, it cannot be regenerated in the central nervous system. While myelin can repair itself, the nerve fiber itself does not regrow. That’s why preventing damage early is so critical. Current treatments aim to slow degeneration, not restore lost function.
Why do some people with MS get worse even when they’re not having relapses?
Because the disease shifts from inflammation to neurodegeneration. In progressive MS, damage comes from inside the brain-microglia, mitochondrial failure, and sodium overload-not from new immune attacks. MRI scans may show no new lesions, but nerves are still dying slowly. This is why disability keeps climbing even without flare-ups.
Are disease-modifying therapies effective for progressive MS?
Most DMTs were designed for relapsing MS and work poorly in progressive stages. Ocrelizumab and siponimod are the only two approved for certain forms of progressive MS, and they only slow decline by about 25%. They don’t stop progression. New drugs targeting nerve protection are in trials but not yet available.
Does brain atrophy mean I’m getting worse?
Yes. Brain atrophy, especially in gray matter, is one of the strongest predictors of future disability. A 2023 study found that patients with faster brain volume loss over 4 years were 3 times more likely to need a cane within 6 years. Standard MRI misses this. Ask for a volumetric scan-it’s more telling than lesion count.
What lifestyle changes have the biggest impact on slowing MS progression?
Quitting smoking has the biggest effect-smokers progress 3 times faster. Regular aerobic exercise (like walking or swimming) boosts nerve-protective proteins. Maintaining vitamin D levels above 40 ng/mL reduces relapse risk and slows atrophy. These aren’t optional extras-they’re essential parts of long-term MS care.