Imagine your body is a car. One warning light comes on - maybe the oil pressure. You fix that. But what if five lights are blinking at once? Oil, temperature, battery, fuel, and brakes? That’s not just a list of problems. That’s a system failure. Metabolic syndrome is exactly that - five warning lights flashing together, signaling your body’s core systems are breaking down in sync. And the biggest danger? It quietly raises your risk of heart disease, stroke, and type 2 diabetes long before you feel sick.
What Exactly Is Metabolic Syndrome?
Metabolic syndrome isn’t one disease. It’s a cluster of five related conditions that happen together and multiply your risk for serious illness. You don’t need all five - just three out of five to be diagnosed. These aren’t random symptoms. They’re signs your body is struggling with insulin, fat, and blood flow in a dangerous way.
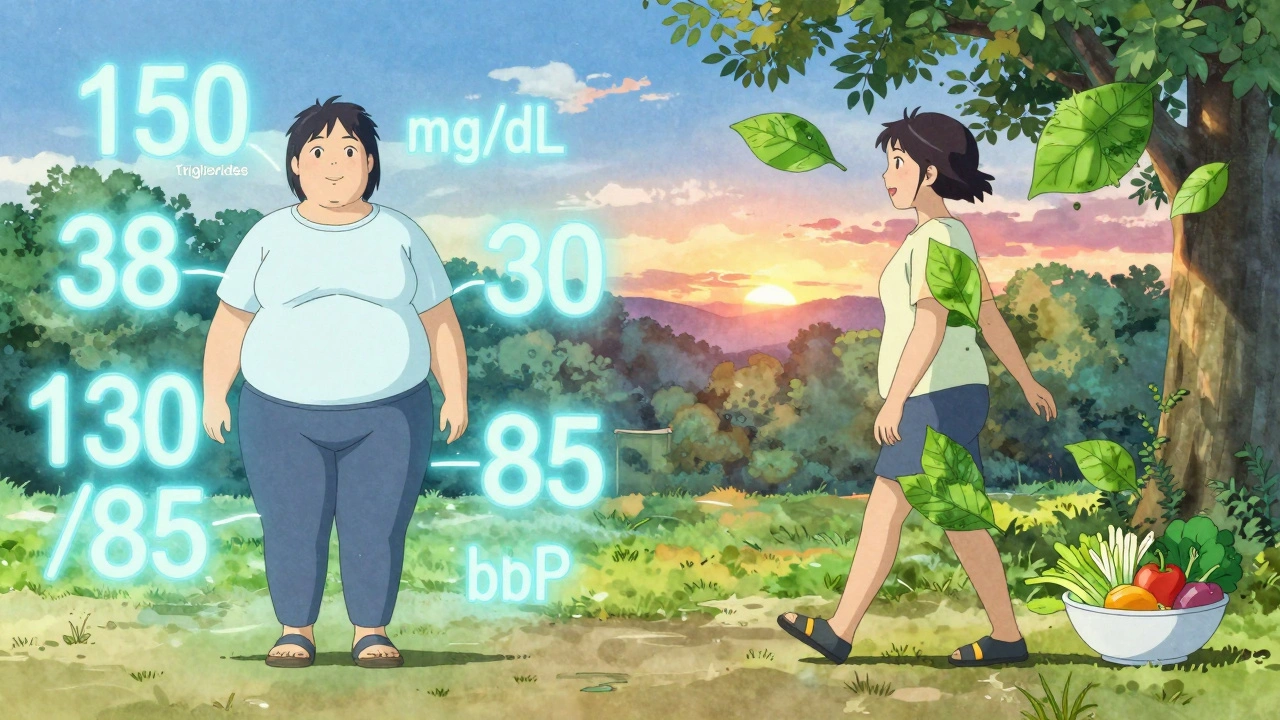
The five diagnostic markers are clear and measurable:
- Abdominal obesity: Waist size over 40 inches (102 cm) for men, or 35 inches (88 cm) for women. For Asian populations, the thresholds are lower - 35 inches for men and 31 inches for women - because fat around the belly becomes dangerous at smaller sizes.
- Elevated triglycerides: 150 mg/dL or higher. This is the fat in your blood that doesn’t clear properly.
- Low HDL cholesterol: Below 40 mg/dL for men, below 50 mg/dL for women. HDL is the "good" cholesterol that cleans out arteries. When it’s low, plaque builds up faster.
- High blood pressure: 130/85 mmHg or higher. Even if it’s just one number up, it’s a red flag.
- Fasting blood sugar: 100 mg/dL or higher. This isn’t diabetes yet - but it’s a loud warning.
According to data from the National Health and Nutrition Examination Survey (NHANES), nearly 35% of U.S. adults have metabolic syndrome. That’s over 86 million people. And the numbers keep rising - especially in people over 60, where it affects almost half the population.
Why This Cluster Is Worse Than Any Single Risk Factor
Having high blood pressure alone is bad. Having high cholesterol alone is bad. But when they show up together - along with belly fat and insulin resistance - the damage isn’t just added. It’s multiplied.
The real villain here is insulin resistance. Your body’s cells stop responding properly to insulin, the hormone that moves sugar from your blood into your muscles and fat for energy. So your pancreas pumps out more insulin to compensate. That excess insulin doesn’t just raise blood sugar - it triggers inflammation, makes your liver churn out more fat, and causes your blood vessels to stiffen.
This creates a cycle: belly fat releases fatty acids directly into your liver, which worsens insulin resistance. Higher insulin pushes your kidneys to hold onto sodium, raising blood pressure. It also lowers HDL and raises triglycerides. It’s not five separate problems. It’s one broken system with five visible symptoms.
Studies like the Framingham Heart Study show people with metabolic syndrome have 1.5 to 2 times the risk of heart disease and five times the risk of developing type 2 diabetes compared to those with none of the risk factors. The American Heart Association confirms that metabolic syndrome gives doctors a clearer picture of future risk than looking at any single number alone.
Why Doctors Miss It - And Why That’s Dangerous
Here’s the problem: most doctors treat individual numbers, not the pattern.
You go in for a checkup. Your blood pressure is high. They prescribe a pill. Next visit, your triglycerides are up. They give you a statin. Your glucose is borderline - they tell you to "watch your sugar." But no one connects the dots. A 2022 survey on HealthUnlocked found that 68% of people with metabolic syndrome weren’t diagnosed because their doctors focused on one issue at a time.
It’s like fixing a flat tire on a car that’s also leaking oil, has worn brakes, and a failing alternator - and calling it a day. The car will still break down. And so will your body.
People with conditions like polycystic ovary syndrome (PCOS) are especially vulnerable. Hormonal imbalances make insulin resistance worse, and many don’t realize their weight gain, acne, and irregular periods are part of the same metabolic problem.
The Only Proven Treatment: Lifestyle - Not Pills
There is no drug approved specifically to treat metabolic syndrome as a whole. That’s not an accident. The solution isn’t a pill - it’s a lifestyle overhaul.
The Diabetes Prevention Program (DPP), one of the most important studies in modern medicine, proved this. People at high risk for diabetes who lost 7% of their body weight through diet and 150 minutes of walking per week reduced their risk of developing metabolic syndrome by 41% over 10 years. That’s more effective than any medication.
What does that look like in real life?
- Weight loss: Losing just 5-10% of your body weight can reverse two or more risk factors. A man weighing 220 pounds who loses 15 pounds can drop his waist size, blood pressure, and blood sugar significantly.
- Exercise: 30 minutes of brisk walking, cycling, or swimming five days a week. You don’t need to run a marathon. Consistency matters more than intensity.
- Diet: Cut out sugary drinks, refined carbs (white bread, pastries, pasta), and processed snacks. Focus on vegetables, lean proteins, whole grains, nuts, and healthy fats like olive oil and avocado. Aim for 1,200-1,500 calories a day for women, 1,500-1,800 for men.
Real people are seeing results. Reddit users in r/MetabolicSyndrome report losing an average of 7.3% of their body weight in six months - and seeing one or two risk factors disappear. One man in Sydney dropped his waist from 44 inches to 36 inches in nine months just by walking daily and cutting soda. His blood pressure went from 142/90 to 118/76. He didn’t need medication.
What’s New in Treatment - And What’s Coming
Science is catching up. In January 2023, the FDA approved the first digital therapeutic for metabolic syndrome: the DarioHealth Metabolic+ app. It uses continuous glucose monitoring and AI coaching to help users adjust their diet in real time. In a trial, users saw their HbA1c drop by 0.6% and waist size shrink by over 3 cm in just six months.
Researchers are also identifying genetic markers like PNPLA3 and TM6SF2 that predict who responds best to certain diets or exercise routines. This could lead to personalized plans - not one-size-fits-all advice.
The American College of Cardiology now says metabolic syndrome is a "risk enhancer" - meaning if you have it, you should start statins earlier than you otherwise would. That’s a shift in thinking: we’re not just treating numbers anymore. We’re treating the whole pattern.

The Bigger Picture: A Growing Global Crisis
Metabolic syndrome isn’t just an American problem. The Global Burden of Disease Study predicts nearly 40% of the world’s adults will have it by 2030. The biggest spikes are happening in South Asia and Latin America - places where diets are shifting toward processed foods and physical activity is declining.
In the U.S., the cost is staggering: $219 billion a year in medical bills, plus $143 billion in lost work time. And it’s not evenly spread. Hispanics have the highest prevalence at 38.6%, followed by non-Hispanic whites at 34.2%. But the good news? It’s one of the most preventable conditions on the planet.
The DiRECT trial in the UK showed that with intensive weight loss - 15 kg or more - 46% of people with type 2 diabetes and metabolic syndrome went into remission. Their blood sugar returned to normal. Their blood pressure dropped. Their triglycerides fell. They didn’t just manage the syndrome - they reversed it.
What You Can Do Right Now
You don’t need a doctor’s order to start fixing this. Here’s your action plan:
- Measure your waist. Stand up, relax, and wrap a tape measure around your belly at the level of your navel. If it’s over 40 inches (men) or 35 inches (women), you’re in the danger zone.
- Get your numbers checked. Ask your doctor for a fasting lipid panel, fasting glucose, and blood pressure readings over a week. Don’t rely on one visit.
- Start walking. Just 30 minutes a day, five days a week. Park farther away. Take the stairs. Walk after dinner.
- Stop drinking sugar. Soda, juice, sweetened coffee, energy drinks - they’re liquid fat. Replace them with water, unsweetened tea, or sparkling water.
- Focus on whole foods. Eat more vegetables, beans, eggs, fish, nuts, and plain yogurt. Cut back on packaged snacks, white rice, and bread.
You don’t have to be perfect. You just have to start. And you don’t need to do it alone. Community programs like the CDC’s National Diabetes Prevention Program use trained coaches - often lay health workers - to help people stick with it. In one study, Hispanic participants lost more weight with this support than with standard care.
Final Thought: This Is Your Body’s SOS
Metabolic syndrome isn’t a diagnosis you ignore. It’s your body screaming for help - before a heart attack, stroke, or diabetes diagnosis hits. It’s not about being "fat" or "lazy." It’s about how modern food, stress, and inactivity have rewired your metabolism.
The good news? You can turn it around. Not with a miracle drug. Not with surgery. But with real, consistent changes to how you move, eat, and live. The science is clear. The proof is in the numbers. And the time to act is now - before the next warning light comes on.



Suzanne Johnston
December 11, 2025 AT 05:58Metabolic syndrome isn’t just a medical diagnosis-it’s a cultural symptom. We’ve built a world that rewards speed, convenience, and numbness, then act shocked when the body rebels. The real question isn’t why people get it-it’s why we keep treating symptoms like isolated bugs instead of systemic crashes. We fix the oil light but ignore the fact the whole engine’s been running on sugar and stress for decades.
Graham Abbas
December 12, 2025 AT 03:21I love this analogy of the car with five warning lights. It’s so much more vivid than medical jargon. I’ve seen friends get prescribed five different pills for five different numbers, and they’re just more confused and tired. But when you frame it as a system failure? Suddenly it clicks. The body’s not broken-it’s begging for a reset. And that reset is just walking, eating real food, and sleeping. Simple. Not easy. But simple.
ian septian
December 12, 2025 AT 04:19Walk more. Cut soda. Sleep better. That’s it. No magic. Just consistency.
Haley P Law
December 13, 2025 AT 05:13OMG YES THIS IS SO TRUE 😭 I lost 12 lbs in 3 months just by swapping soda for sparkling water and walking after dinner. My waist went from 41 to 35. My doc was like ‘wait did you do something??’ I was like ‘nope just stopped drinking liquid candy’ 🙃
Steve Sullivan
December 14, 2025 AT 08:50they say its about insulin resistance but honestly i think big pharma just dont want us to know that the real fix is free and doesnt involve their pills. why else would they ignore the fact that 7% weight loss cuts risk by 41%? because that’s not profitable. they want you dependent. they want you taking statins, metformin, blood pressure meds forever. the truth? you can reverse this with food and movement. but that’s not on the label.
Andrea Petrov
December 15, 2025 AT 03:33Let’s be real-this whole ‘lifestyle change’ narrative is just a way to blame the victim. What about food deserts? What about people working three jobs and living in neighborhoods where the only ‘healthy’ option is a gas station with expired kale? And don’t even get me started on how ‘exercise’ is a luxury when you’re chronically exhausted from systemic stress. This article sounds like it was written by someone who’s never missed a meal or worked a night shift. You can’t ‘walk more’ when your body’s in survival mode. Stop pretending this is about willpower.
Suzanne Johnston
December 16, 2025 AT 17:54Andrea makes a valid point. The systemic neglect of public health infrastructure is what allows metabolic syndrome to flourish. We don’t lack knowledge-we lack equity. A person in Detroit with no access to fresh produce and a 60-hour workweek isn’t failing because they’re lazy. They’re failing because the system failed them. The solution isn’t individual discipline-it’s policy change: subsidized healthy food, paid time off for wellness, urban design that encourages movement. Until then, telling people to ‘just walk’ is like telling someone in a sinking boat to swim harder.
Chris Marel
December 16, 2025 AT 19:37as someone from nigeria where processed food is now cheaper than yam and plantain, i see this everywhere. people think its ‘western disease’ but no-it’s a global disease of convenience. my uncle had all five markers at 48, worked as a taxi driver, ate mostly fried plantain and sugary tea. he didn’t know it was connected. no one told him. the system doesn’t care until you’re in the hospital. we need community health workers-not just apps.
George Taylor
December 16, 2025 AT 20:07...and yet, despite all this data, the CDC still recommends ‘moderate physical activity’... which is vague, unmeasurable, and utterly useless for the 70% of people who don’t know what ‘moderate’ even means. Also, the DarioHealth app? Paid subscription. $30/month. For a system that’s supposed to be ‘preventable’? That’s a joke. You’re selling hope to the poor while the rich get personalized DNA diets. This isn’t medicine. It’s capitalism with a stethoscope.
Anna Roh
December 18, 2025 AT 09:29my dad had metabolic syndrome and died of a heart attack at 59. he was told to ‘eat less’ and ‘walk more’ but never got real guidance. the system fails people like him every day. no one taught him how to cook. no one helped him find time. no one listened. now i’m 32 and i see the same patterns in my friends. it’s not about willpower. it’s about being left alone to figure out a system designed to break you.
Carina M
December 18, 2025 AT 13:03It is both disconcerting and profoundly disheartening to observe the pervasive tendency within contemporary discourse to reduce complex physiological phenomena to simplistic, populist platitudes. The notion that metabolic syndrome can be remediated through mere ‘walking’ and ‘cutting soda’ is not merely reductive-it is epistemologically negligent. One must consider the intricate neuroendocrine, genetic, and epigenetic underpinnings that defy such banal interventions. To suggest otherwise is to engage in medical populism of the most dangerous variety.