The FDA doesn’t just check labels or packaging. It digs into the manufacturing process-the real heart of drug and device safety. In 2025, warning letters from the FDA revealed a troubling pattern: the same basic failures keep showing up, again and again, putting patients at risk. These aren’t random mistakes. They’re systemic breakdowns in how companies manage quality. And the FDA is responding with more inspections, tougher penalties, and a new focus on culture, not just paperwork.
Aseptic Processing Failures: The Silent Killer
One in every two warning letters in 2025 cited problems with aseptic processing. That’s the method used to make injectable drugs, IV solutions, and sterile medical devices without letting bacteria or viruses in. If this step fails, the product can kill people.
The FDA found facilities where workers didn’t properly validate their sterile environments. Media fill studies-simulations that test whether contamination can creep in during production-were either missing or flawed. In one case, a company used a glove box that wasn’t sealed correctly. In another, staff skipped gowning procedures because they were rushed. These aren’t minor oversights. They’re direct paths to deadly infections.
The FDA expects companies to prove sterility isn’t just luck. It requires repeated testing, environmental monitoring, and training that’s documented and followed. When these controls are ignored, the FDA doesn’t just issue a warning. It blocks the product from entering the U.S. market.
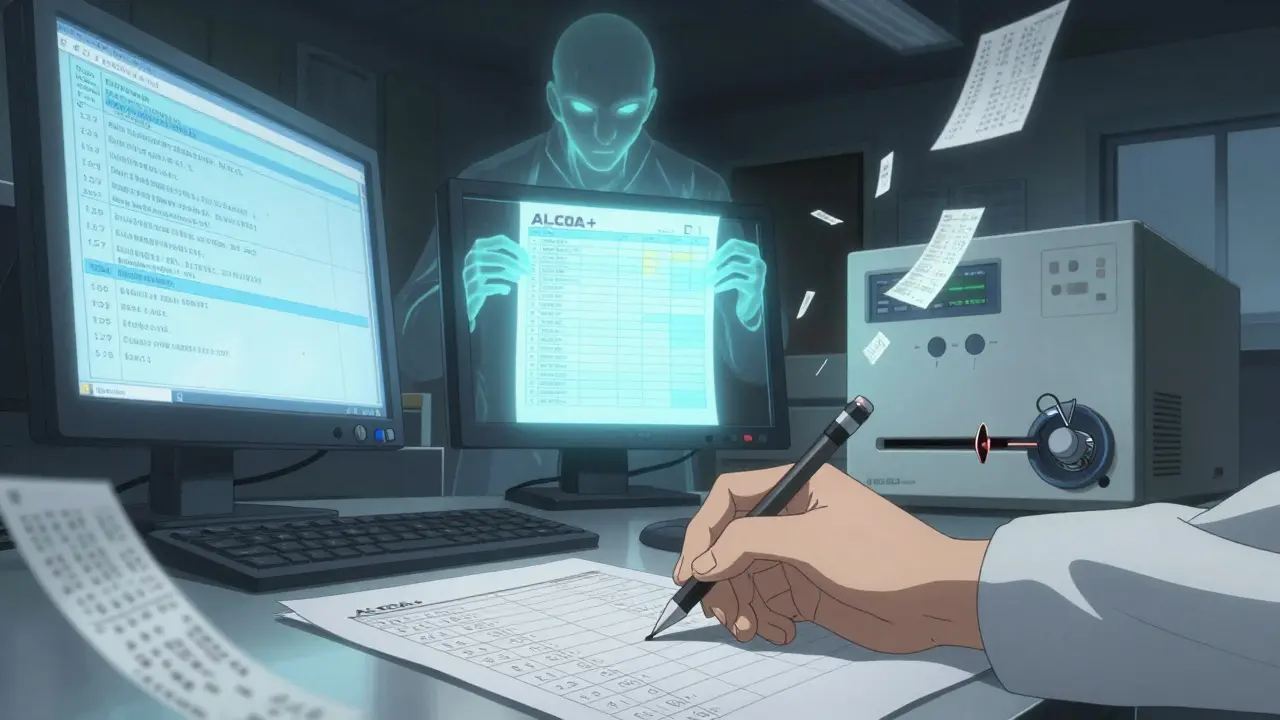
Data Integrity: When the Records Don’t Match Reality
Thirty-nine percent of 2025 warning letters targeted data integrity failures. This means the records didn’t reflect what actually happened on the factory floor. Some companies used erasable pens to correct batch records. Others deleted electronic logs or turned off audit trails on testing instruments like UV-Vis spectrometers.
The FDA’s ALCOA+ standard isn’t optional. Data must be:
- Attributable
- Legible
- Contemporaneous
- Original
- Accurate
- Plus complete, consistent, enduring, and available
One Chinese manufacturer was caught using laminated sheets with pencil notes-easily changed, never traceable. Another deleted raw data after passing a test, claiming it was "redundant." The FDA doesn’t accept that. Every test result, every adjustment, every correction must be recorded and preserved for at least 180 days. Electronic systems must lock users out if they try to delete data. No exceptions.
Material Control: Dangerous Ingredients Slip Through
Bad raw materials can turn a safe product into a poison. In 2025, the FDA found multiple cases where suppliers weren’t properly vetted, and incoming materials weren’t tested for deadly contaminants.
One company used glycerin in its toothpaste that hadn’t been checked for diethylene glycol (DEG)-a toxic chemical linked to kidney failure. Another didn’t verify whether its sorbitol supplier was testing for ethylene glycol (EG). Both are common industrial solvents that can accidentally contaminate pharmaceutical ingredients if the supply chain isn’t tightly controlled.
The FDA requires manufacturers to test high-risk materials using validated methods. For DEG and EG, that means testing down to 0.1% concentration, as outlined in USP <1085>. Supplier audits aren’t optional. You can’t just trust a certificate of analysis. You have to prove the supplier’s testing is reliable. That means on-site visits, sample retesting, and documented agreements.
Process Validation: Making Things Work-Consistently
Just because a product works once doesn’t mean it will work every time. That’s why process validation is required. In 2025, 28% of warning letters cited missing or incomplete validation studies.
One company made toothpaste in large batches but never tested whether the mixing process evenly distributed active ingredients. Another used a new tablet press but didn’t prove it could consistently hit the right hardness and dissolution rate. The FDA expects three consecutive successful batches under normal production conditions, with every step monitored and recorded.
Validation isn’t a one-time task. It’s an ongoing commitment. If you change a machine, a supplier, or a formula, you must revalidate. Skipping this step means your product’s quality is guesswork-and the FDA treats guesswork as a violation.
Quality Culture: The Root Cause Behind Every Failure
Behind every data entry error, every skipped test, every unvalidated process is a deeper problem: culture. According to experts analyzing 2025 warning letters, 78% of facilities showed leadership that prioritized speed over compliance.
Managers pushed teams to meet deadlines even when controls weren’t ready. Quality teams were underfunded and had no authority to stop production. Employees were afraid to speak up. One company admitted in its response letter: "This site does not prepare batch production records for every batch of our listed drug." That’s not incompetence. That’s indifference.
The FDA’s new Quality Management Maturity (QMM) program, launched in early 2024, is designed to catch this. It doesn’t just check boxes. It asks: Does leadership own quality? Are employees trained to stop the line? Is quality measured in metrics, not just audits?
Companies that fix their culture see 63% fewer repeat violations. The FDA is now using QMM results to decide who gets inspected more often-and who gets a break.
Where Are These Problems Happening?
While violations occur globally, patterns are clear. In 2025:
- Chinese facilities were cited 28 times for poor analytical method validation
- Indian facilities saw 24 warnings for data integrity failures
- Malaysian sites were flagged 9 times for weak quality unit authority
The FDA increased unannounced inspections by 40% in 2025, and 68% of those targeted facilities in Asia. Many of these companies had never been inspected before. Now, they’re on Import Alert 66-40-meaning their products are blocked from entering the U.S. until they prove they’ve fixed the issues.
Even domestic U.S. facilities aren’t safe anymore. The FDA plans to conduct 1,200 unannounced inspections in 2026-up from 850 in 2025. No one is exempt.
What Happens When You Get a Warning Letter?
Getting a warning letter isn’t the end-but it’s the start of a long, expensive road. In 92% of 2025 cases, the FDA required companies to hire an independent CGMP consultant. The average remediation time? 6 to 18 months.
Fixing data integrity? You need validated audit trails, user access controls, and 180-day record retention. Fixing aseptic issues? You need full media fill studies, environmental monitoring, and staff retraining. Fixing material controls? You need supplier audits and validated testing protocols.
And it’s not just about fixing the problem. You have to prove it won’t happen again. That means new training programs, updated SOPs, and internal audits that actually find issues before the FDA does.
What’s Next for Manufacturers?
The FDA’s focus is shifting. It’s no longer just about checking if you followed the rules. It’s about whether you have a culture that makes compliance automatic.
Emerging areas of scrutiny include:
- Cloud-based quality systems-12 warning letters in 2025 cited poor controls
- Contract labs-8 letters found insufficient oversight of outsourced testing
- Continuous manufacturing-5 letters questioned validation of new tech
Spending on compliance solutions hit $4.7 billion in Q3 2025. That’s up 12.3% from last year. Companies are realizing: paying for quality now is cheaper than getting shut down later.
The message is clear: if your manufacturing process isn’t built on science, transparency, and accountability, you’re not just at risk of a warning letter. You’re risking lives-and your business.
What are the most common FDA manufacturing violations in 2025?
The top three violations in 2025 were aseptic processing failures (47% of warning letters), data integrity issues (39%), and material control lapses (35%). These include unvalidated sterile environments, missing audit trails, and untested raw materials like glycerin for toxic contaminants.
Can a company fix an FDA warning letter without a consultant?
Technically, yes-but in practice, almost no one does. The FDA required independent CGMP consultants in 92% of 2025 warning letters. Internal teams rarely have the objectivity or expertise to fix systemic failures. The FDA expects an outside expert to validate the fix.
Why does the FDA care about quality culture?
Because technical fixes don’t last if the culture doesn’t change. If leadership rewards speed over compliance, employees will cut corners again. The FDA’s QMM program shows that companies with strong quality cultures have 63% fewer repeat violations and fix problems 41% faster.
Are U.S. manufacturers being inspected more now?
Yes. In 2026, the FDA plans 1,200 unannounced inspections of domestic facilities-up from 850 in 2025. No company, domestic or foreign, is exempt. The era of scheduled inspections is over.
What happens if a product is placed on Import Alert 66-40?
The product is automatically detained at the U.S. border. It can’t enter the country unless the company submits a detailed corrective action plan and proves compliance through physical examination by FDA inspectors. This can take months and cost hundreds of thousands of dollars.



Todd Scott
December 27, 2025 AT 16:04Man, I've seen this play out in pharma ops before. Aseptic failures aren't just about gloves or clean rooms-they're about leadership turning a blind eye when production is behind. I worked at a mid-size injector plant where the QA lead got pushed out for 'being too slow.' Two months later, we had a recall because of endotoxins in a batch that never got tested. The FDA doesn't care if you're busy. They care if you're lying to yourself.
And don't even get me started on data integrity. I once saw a lab tech use a highlighter to 'correct' a chromatogram peak. Said it was 'just for clarity.' The audit trail was disabled because 'it slowed things down.' That's not incompetence. That's cultural rot. The QMM program is long overdue. You can't audit your way out of a toxic culture.
Also, cloud-based quality systems? Yeah, I've seen those fail too. One company used a SaaS platform that auto-deleted logs after 30 days. They thought it was 'cost-efficient.' The FDA found out because a whistleblower sent them a screenshot from a personal phone. Never underestimate the guy who still prints out his batch records.
And let's be real: no one's getting inspected unless they're already on the radar. The 40% increase in unannounceds? That's not random. That's targeted. They're following the money-where the cheapest APIs are coming from, where the turnover is highest, where the managers still say 'we've always done it this way.'
Fixing this isn't about buying new software. It's about hiring people who won't shut up when something's wrong. And then listening to them.
Also, DEG in glycerin? That's been a known risk since the 90s. If you're still missing that, you're not cutting corners. You're just not trying.
And yes, consultants are expensive. But so is a shutdown. And a lawsuit. And a dead patient.
Satyakki Bhattacharjee
December 28, 2025 AT 07:57This is what happens when people forget God's law. The FDA is just a tool of the elite to control the poor. Why do you think they target India and China? Because they are hardworking nations who feed the world with medicine. The real problem is Western greed. They want to charge $1000 for a pill that costs $2 to make. They call it 'quality' but it's just profit. The workers are not to blame. The system is broken.
Let the people make medicine. Let them use pencils. Let them work fast. God will protect the innocent.
Anna Weitz
December 29, 2025 AT 17:35So let me get this straight-you're telling me the FDA is suddenly concerned about patient safety after letting this go on for decades? They're the ones who approved tons of these companies in the first place. They're the ones who gave out certifications while ignoring red flags. Now they want us to believe they're the moral police? Please. This is theater. They need to justify their budget. They need to scare companies into paying more for compliance consultants. The real issue? Corruption. The same people who wrote the guidelines are now getting paid to audit them. It's a closed loop. And you're all just falling for it.
And don't even get me started on 'quality culture.' That's corporate speak for 'obey without question.'
Real quality? It's when you make something good because you care. Not because you're scared of a letter.
Babe Addict
December 30, 2025 AT 20:39Let’s cut through the FDA propaganda. Aseptic processing? It’s a myth. You can’t sterilize air. You can’t sterilize humans. The entire ISO 14644 framework is based on 1970s assumptions. The real solution is lyophilization or single-use systems. But no-everyone’s still chasing laminar flow hoods because that’s what the GMP checklist says. Data integrity? Please. Every single lab has a workaround. The FDA knows it. They just want you to pay for the audit trail software so they can fund their next budget cycle.
And 'quality culture'? That’s HR jargon for 'stop asking questions.' The moment you tell your team to stop the line, you’re asking them to risk their jobs. That’s not culture-that’s fear. The FDA doesn’t want culture. They want compliance theater. And the consultants? They’re the real winners. They make more money off your panic than you make off your product.
Also, 68% of inspections in Asia? That’s not science. That’s xenophobia. They don’t inspect U.S. facilities the same way. Ever notice that? The same violation gets a 'notice of opportunity to respond' in Ohio and a detention order in Bangalore. Double standard. Always has been.
Chris Garcia
December 31, 2025 AT 07:13There is a profound truth buried beneath these regulatory bulletins: the erosion of human dignity in the name of efficiency. When a worker skips gowning because they are rushed, it is not merely a procedural lapse-it is the quiet death of reverence for life. The sterile environment is not a machine to be calibrated; it is a sacred space where human hands must be humble before the sanctity of the body they serve.
And when data is erased, it is not just a file that vanishes-it is the memory of responsibility, the echo of conscience. The ALCOA+ principle is not a checklist; it is a covenant. Attributable? Yes. But more importantly, accountable. Legible? Yes. But more importantly, honest. Contemporaneous? Yes. But more importantly, faithful.
The Chinese manufacturer with pencil notes on laminated sheets? He was not a criminal. He was a man caught in a system that demanded perfection but offered no dignity. The Indian lab that deleted raw data? He was not a cheat. He was a soul crushed under the weight of deadlines no human could meet.
The FDA’s QMM program, for all its flaws, at least acknowledges this: quality is not engineered. It is cultivated. In soil watered by respect. In hearts nourished by trust. Until leadership stops treating compliance as a cost center and starts treating it as a calling, no software, no audit, no consultant will save us.
Let us not merely fix processes. Let us restore humanity.
Liz Tanner
January 1, 2026 AT 19:38I’ve worked in pharma QA for 18 years. I’ve seen the good, the bad, and the ugly. And honestly? Most of these violations aren’t from evil people. They’re from exhausted people. People who’ve been told to do more with less for years. People who’ve been yelled at for slowing down production. People who know the right thing to do but don’t have the power to do it.
And yeah, some are lazy. Some are dishonest. But the majority? They just want to go home at the end of the day without someone getting sick.
The FDA’s new focus on culture? That’s the first real step they’ve taken in a decade. Because you can’t audit your way out of a culture that rewards silence. You need to empower the person on the floor to say ‘stop.’ You need to train managers to listen. You need to reward honesty, not just compliance.
And for the love of God, stop using erasable pens. Just use a digital system. It’s 2025. We’re not in the 1980s anymore.
Also-supplier audits? Do them. Don’t just take a COA. Go see it yourself. One time I flew to a supplier in Malaysia just to watch them test a raw material. Turned out their lab was using expired reagents. Saved us from a recall. Worth every penny.
Quality isn’t a department. It’s a mindset. And it starts with listening.
Liz MENDOZA
January 2, 2026 AT 15:12My cousin works in a plant in India. She told me they’re told to 'get it done' every single day. No one ever says 'take your time.' No one ever says 'if you’re not sure, stop.' She’s terrified to speak up because last time she asked a question, they moved her to night shift for a month.
I just want to say-this isn’t just about regulations. It’s about people. Real people. With families. With fears. With hopes. The FDA’s QMM program? It’s the first thing I’ve seen that actually tries to fix that.
Let’s not just punish. Let’s support. Let’s train. Let’s listen. Because the people making the medicine? They’re not the enemy. They’re the ones who need us the most.
Jane Lucas
January 4, 2026 AT 04:59so like i was reading this and i just kept thinking… why are we still using all these manual processes in 2025? like why are people writing things down with pencils?? like just use a tablet and lock the data. its not that hard. and why do companies still hire people who dont know how to use a computer?? like come on.
also i think the FDA is kinda late to the party but hey better late than never i guess
dean du plessis
January 5, 2026 AT 18:41Interesting read. I’m from South Africa and we’ve had our own issues with medicine quality, especially with generics. But what strikes me is how little we talk about the human side. The guy who’s skipping gowning because he’s got three kids to feed and no sick days. The lab tech who deletes data because he’s been working 14-hour shifts for a month. The system’s broken. The FDA’s response is a start. But real change? That’s gonna take leadership that actually cares. Not just compliance officers. Real leaders.
Also-why is everyone blaming Asia? The U.S. has had its own scandals. Just look at the opioid crisis. Same culture. Same silence. Same fear.
Kishor Raibole
January 6, 2026 AT 05:37It is with profound sorrow and unyielding resolve that I address this matter. The FDA’s warning letters are not mere administrative notices-they are the funeral orations of a civilization that has abandoned its moral compass in the altar of profit. The aseptic failures? They are the cries of the dying, silenced by the machinery of indifference. The data integrity breaches? They are the erasure of truth itself, committed not by malice, but by the cold calculus of corporate expediency.
And yet, we are told to ‘fix the culture.’ As if culture were a switch to be toggled. As if the soul of a factory could be rewired with a PowerPoint presentation.
What is required is not training. Not software. Not even audits.
It is repentance.
Repentance from the executives who have turned medicine into a commodity. Repentance from the regulators who have looked away. Repentance from the consumers who have accepted the illusion of cheapness.
Until we restore reverence to the act of healing, no warning letter will suffice. No consultant will heal. No inspection will save us.
Let this be the hour of reckoning.
John Barron
January 6, 2026 AT 07:27Okay but let’s be real-this whole thing is a scam. The FDA doesn’t care about safety. They care about funding. Every time they scare the industry, Congress gives them more money. That’s why they’re pushing QMM. It’s a new revenue stream. Consultants? They’re paid by the hour. Software vendors? They’re selling $500k systems for something that should be a $50 plugin.
And the ‘culture’ stuff? That’s just corporate buzzword bingo. ‘Psychological safety’? ‘Ownership’? Please. The real problem is that the FDA is still using paper forms in 2025. How can they audit digital systems if their own tech is from 2008?
Also-why are they only inspecting Asia? Because they’re scared to look at U.S. plants. They know they’d find the same crap here. It’s a distraction. A smokescreen. And we’re all falling for it.
Also 🤡
Elizabeth Alvarez
January 6, 2026 AT 09:53Have you ever wondered why all these violations are happening in places with large immigrant workforces? Coincidence? I don’t think so. The FDA’s crackdown on Asian manufacturers? It’s not about safety. It’s about control. The same people who pushed for offshoring are now screaming about quality. They knew this would happen. They planned it. This is how they justify bringing manufacturing back to the U.S.-by making foreign factories look like death traps.
And the ‘quality culture’? That’s just code for ‘stop trusting foreign workers.’ They want U.S.-based employees who won’t question authority. Who won’t unionize. Who’ll work for minimum wage and say nothing.
And the consultants? They’re all connected. Same firms. Same clients. Same lobbying groups. This whole system is rigged. The FDA isn’t protecting patients. They’re protecting the pharmaceutical oligopoly.
And don’t even get me started on cloud-based systems. Your data is being sold. Every audit trail is tracked. Your company’s secrets? They’re already in the hands of third-party vendors. And you think that’s safe?
Wake up. This isn’t about medicine. It’s about power.
Miriam Piro
January 7, 2026 AT 22:32Okay but what if… the FDA is lying? What if they’re the ones contaminating the samples? I read this one whistleblower blog from 2023-some ex-FDA inspector said they were told to ‘adjust’ environmental monitoring results to make facilities look worse than they were. Why? To justify more inspections. More funding. More contracts for their friends in consulting.
And the ‘unannounced’ inspections? They’re not unannounced. They’re scheduled. The companies get a heads-up. They clean up. They fake the records. The FDA knows. They just don’t say anything because they need the drama to keep their budget.
Also-why do all the warning letters come from the same 5 labs? Coincidence? Or are those labs owned by the same parent company that sells the audit software?
And the QMM program? It’s a front. They’re not measuring culture. They’re measuring compliance with their proprietary framework. The companies that pass? They’re the ones who paid the most for the training.
Wake up. The system is a pyramid scheme. And we’re all paying for it.
Also 🤫👁️👁️
Kylie Robson
January 8, 2026 AT 13:41Let’s not conflate GMP with quality. GMP is a regulatory framework. Quality is a scientific discipline. The FDA treats them as synonyms. They’re not. Process validation isn’t about three batches-it’s about statistical process control, capability indices, and risk-based sampling. If you’re doing media fills based on ISO 14644 Class 8 instead of real-time particle monitoring, you’re not compliant-you’re playing pretend.
And data integrity? ALCOA+ is a good start, but it’s not enough. You need metadata integrity, electronic signatures with biometric binding, and blockchain-backed audit trails. If your LIMS doesn’t have NIST-traceable time stamps, you’re not just non-compliant-you’re vulnerable to tampering.
Also-why are we still talking about pencil notes? That’s a 2010 problem. The real issue is AI-generated batch records. Companies are using LLMs to auto-generate SOPs and test results. The FDA hasn’t even begun to address that. And when they do? It’ll be too late.
Bottom line: we’re using 1980s regulatory thinking to manage 2025 manufacturing. That’s why we keep failing. Fix the framework. Not the people.
Anna Weitz
January 10, 2026 AT 08:14And yet, the very people who scream about culture are the same ones who fire the QA lead who speaks up. So who’s really responsible? The worker who skips a step? Or the manager who created the environment where skipping is the only way to survive?
Stop blaming the bottom. Fix the top.