LPV/r Drug Interaction Checker
Check if your medications interact dangerously with Lopinavir/Ritonavir (LPV/r). Enter a drug name to see interaction risks based on the Liverpool HIV Interactions Database.
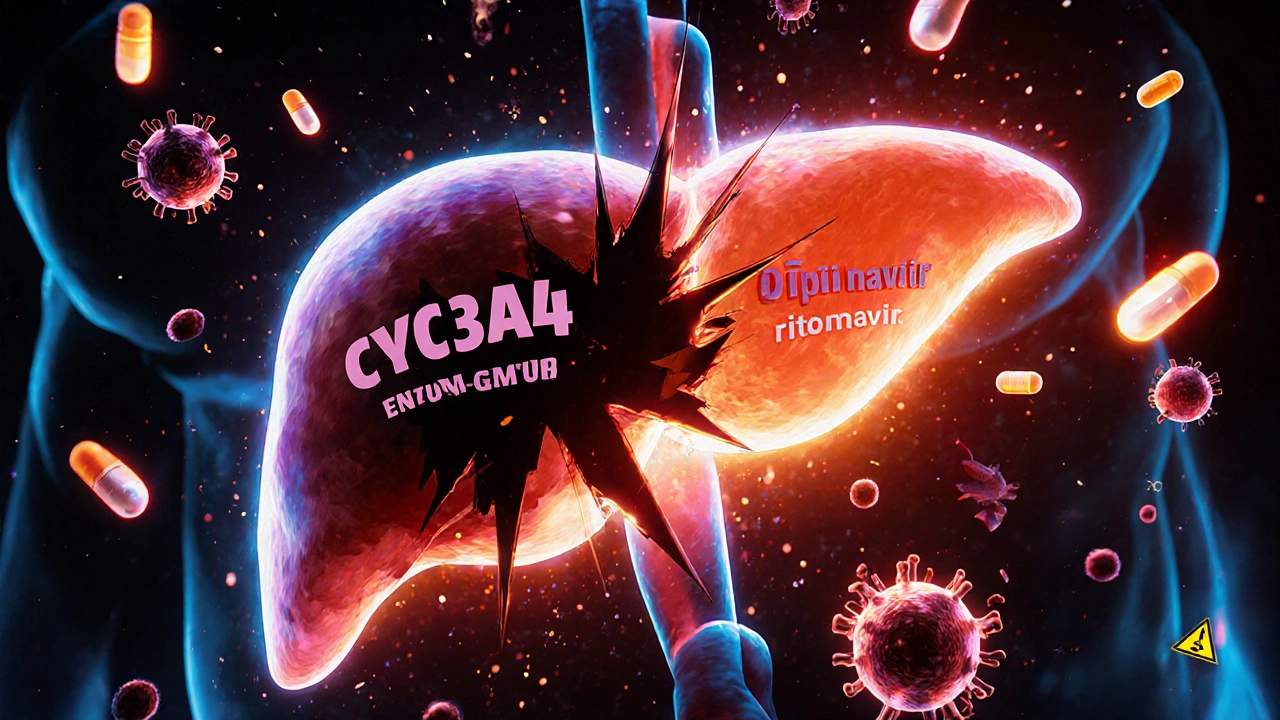
Lopinavir/ritonavir (LPV/r) isn't just another HIV drug combo. It's a pharmacological hack - using a low dose of ritonavir to force the body to keep lopinavir active longer. This trick, called boosting, works because ritonavir shuts down CYP3A4, the main liver enzyme that breaks down lopinavir. Without ritonavir, lopinavir gets cleared too fast to be effective. With it, lopinavir levels stay high enough to suppress HIV - but this same mechanism turns LPV/r into one of the most dangerous drugs for interactions in clinical use.
How Ritonavir Boosts Lopinavir - And Why It’s So Powerful
Lopinavir, on its own, has a half-life of just under 7 hours. That means if you took it without ritonavir, you’d need to dose it three times a day to keep HIV in check. But ritonavir changes everything. At just 100 mg - about 16 times less than the lopinavir dose - it cuts lopinavir’s clearance by more than 85%. This turns a twice-daily regimen into a viable option, improving adherence and reducing side effects tied to high, fluctuating drug levels.
The science behind it isn’t simple inhibition. Ritonavir doesn’t just block CYP3A4 temporarily. It permanently damages the enzyme. Studies show it does this in four ways: it binds tightly to the enzyme’s iron center, destroys its heme group, forms long-lasting complexes, and even sticks reactive fragments directly to the enzyme’s protein structure. This isn’t like flipping a switch - it’s like smashing the tool. Once CYP3A4 is inactivated, it takes days for the liver to make new enzymes. That’s why the effects of ritonavir last far longer than its own presence in the blood.
That’s also why ritonavir is considered the strongest CYP3A4 inhibitor in clinical use. Even cobicistat, designed as a cleaner booster, doesn’t match its depth of inhibition. But this power comes with a price: unpredictability.
The Double-Edged Sword: Inhibition and Induction
Ritonavir isn’t just a CYP3A4 inhibitor. It’s also an inducer - meaning it can speed up the metabolism of other drugs through enzymes like CYP1A2, CYP2B6, CYP2C9, and CYP2C19. This dual nature makes its interaction profile chaotic. One drug might spike in concentration because CYP3A4 is blocked. Another might crash because CYP2C9 is turned up.
Take warfarin, a blood thinner. Ritonavir induces CYP2C9, which breaks down warfarin faster. That means INR levels drop - and patients risk clots. But if you stop ritonavir, warfarin levels can suddenly climb, leading to dangerous bleeding. The same patient might be on midazolam (a sedative) for surgery. Ritonavir blocks its breakdown through CYP3A4, causing levels to jump 500%. One standard dose could cause prolonged unconsciousness or respiratory failure.
These aren’t theoretical risks. In 2008, a study showed that giving rifampicin - a TB drug that induces CYP3A4 - to someone on LPV/r dropped lopinavir levels by 76%. Hepatotoxicity jumped from 11% to 33%. That’s not a side effect. That’s a life-threatening collision.
Real-World Interactions: What Clinicians Actually See
The Liverpool HIV Interactions Database, updated in July 2023, lists 1,247 potential drug interactions with LPV/r. That’s more than 40% of all commonly prescribed medications. Here’s what that looks like in practice:
- Tacrolimus (transplant drug): Levels rise 3-5x. Dose must be cut by 75% or more. Without monitoring, kidney failure or neurotoxicity can occur.
- Rivaroxaban (blood thinner): Contraindicated. The risk of major bleeding is too high.
- Methadone (opioid dependence): Ritonavir induces its metabolism. Dose needs to go up by 20-33%. If missed, withdrawal or overdose can happen.
- Hormonal contraceptives: Ritonavir reduces estrogen levels by 50%. Birth control pills become unreliable. Backup methods aren’t optional - they’re mandatory.
- Voriconazole (antifungal): Unpredictable levels. Sometimes too low (treatment failure), sometimes too high (liver damage). Contraindicated.
Anesthesiologists have their own list. Fentanyl and sufentanil - common painkillers in surgery - can cause fatal respiratory depression when combined with ritonavir. Protocols at major hospitals now require 60-80% dose reductions. One missed adjustment can be deadly.
Why LPV/r Is Still Used - And Where It’s Disappearing
Despite the risks, LPV/r hasn’t vanished. In low- and middle-income countries, it’s still part of 28% of first-line HIV regimens. Why? Cost. In PEPFAR programs, a year of LPV/r costs $68. Newer drugs like dolutegravir cost $287. In places where supply chains are fragile and funding is tight, LPV/r remains a workhorse.
But in the U.S., Europe, and Australia, it’s nearly gone. Since 2015, guidelines have pushed for integrase inhibitors - drugs like dolutegravir and bictegravir - that don’t rely on CYP3A4 boosting. They’re simpler, safer, and have fewer interactions. In the U.S., LPV/r use has dropped below 5%. In Australia, it’s rarely prescribed unless there’s no other option.
Even in HIV, newer boosted regimens like darunavir/cobicistat are preferred. Cobicistat only inhibits CYP3A4 - no induction. Fewer interactions. Fewer surprises.
The COVID-19 Twist: Paxlovid and the Rebound Problem
When the pandemic hit, ritonavir got a second life as part of Paxlovid (nirmatrelvir/ritonavir). The same boosting trick was used to keep nirmatrelvir active long enough to block SARS-CoV-2 replication. It worked - 89% reduction in hospitalization if taken early.
But then came the rebound. Some patients felt better, stopped treatment, and then got sick again days later. Why? Because ritonavir’s inhibition of CYP3A4 lasts longer than nirmatrelvir’s half-life. Once ritonavir clears, CYP3A4 starts coming back online - and suddenly, the body starts breaking down nirmatrelvir again. If viral load wasn’t fully suppressed, it can come roaring back.
This isn’t a flaw in Paxlovid’s design. It’s a feature of ritonavir itself. The same mechanism that makes it a great booster also makes it a lingering disruptor.
What You Need to Do - Step by Step
If you’re prescribing, dispensing, or taking LPV/r, here’s what you must do:
- Check every medication - even over-the-counter drugs, supplements, and herbal products. St. John’s wort? Contraindicated. It induces CYP3A4 and will tank lopinavir levels.
- Use the Liverpool HIV Interactions Database. It’s free, updated monthly, and used by over 2.8 million clinicians annually. Type in any drug - it tells you the risk level and what to do.
- Adjust doses proactively. Don’t wait for symptoms. If a patient is on a statin, reduce the dose. If they’re on methadone, increase it. Document the change.
- Monitor closely. For warfarin: weekly INR for the first month. For tacrolimus: blood levels every 2-3 days after starting LPV/r.
- Never assume safety. Even if a drug isn’t listed as risky, ritonavir’s dual effects can surprise you. When in doubt, hold it.
Who Should Avoid LPV/r Altogether?
Some patients shouldn’t touch it:
- Those on drugs with narrow therapeutic windows (e.g., cyclosporine, quinidine, pimozide)
- Patients with severe liver impairment (Child-Pugh Class C)
- Anyone taking ergot derivatives (risk of gangrene)
- People on alfuzosin (risk of dangerous drops in blood pressure)
- Those who can’t commit to regular lab monitoring
For these patients, integrase inhibitors are the only safe choice.
The Future: Is There a Place for LPV/r?
LPV/r’s days are numbered - but not gone. In places where cost is the only barrier, it will stick around until dolutegravir becomes affordable and accessible. Research is ongoing into how genetic differences in CYP3A5 affect lopinavir levels. Early data shows people who express CYP3A5 clear lopinavir 28% faster. That could mean some patients need higher doses - but only if you test for the gene.
For now, LPV/r remains a powerful tool with dangerous side effects. It’s not a drug you pick because it’s convenient. You pick it only when nothing else works - and you manage it like a live wire.
Can I take ibuprofen with lopinavir/ritonavir?
Yes, ibuprofen is generally safe with LPV/r. It’s metabolized by CYP2C9, but ritonavir’s effect on this enzyme is mild and unpredictable. Still, monitor for stomach upset or kidney strain, especially in long-term users. Avoid high doses or prolonged use without medical supervision.
Why is ritonavir used in such a low dose?
Ritonavir is used at 100 mg - far below its own therapeutic dose - because that’s enough to inhibit CYP3A4 without causing its own side effects like nausea, diarrhea, or liver stress. At full doses (600 mg), ritonavir causes intolerable GI issues. The boosting effect kicks in at just 100 mg, making it a perfect pharmacological tool.
Does ritonavir affect birth control pills?
Yes. Ritonavir reduces estrogen levels by about 50%, making hormonal birth control pills, patches, and rings unreliable. You must use a backup method - like condoms or an IUD - while on LPV/r and for at least 2 weeks after stopping it. This isn’t a suggestion. It’s a medical necessity.
Can I switch from LPV/r to another HIV drug safely?
Yes, but timing matters. Switching to an integrase inhibitor like dolutegravir is common and safe. However, you must wait at least 24-48 hours after the last LPV/r dose to start the new drug. Ritonavir’s effects linger for days, and starting a new drug too soon can cause unpredictable interactions or toxicity. Always consult your HIV specialist before switching.
Is LPV/r still used in Australia?
Rarely. Since 2018, Australian HIV treatment guidelines have recommended integrase inhibitors as first-line. LPV/r is only used in very specific cases - like resistance to newer drugs, or in patients who can’t access or afford alternatives. Most clinics in Sydney and Melbourne no longer prescribe it routinely.


Arun Mohan
November 20, 2025 AT 06:37Wow, this is some next-level pharmacology bullshit. Ritonavir doesn't just inhibit CYP3A4-it surgically murders it like a mob hit on a rival boss. The fact that it permanently damages the enzyme’s structure? That’s not science, that’s alchemy. And people wonder why drug interactions are the #1 cause of hospitalizations in HIV clinics. This isn’t a treatment. It’s a chemical landmine with a timer.
Tyrone Luton
November 20, 2025 AT 11:32It’s ironic, isn’t it? We’ve built a whole medical infrastructure around a molecule that’s essentially a molecular arsonist. Ritonavir doesn’t just boost lopinavir-it hijacks the body’s entire metabolic identity. We’re not treating HIV anymore. We’re negotiating with a biochemical warlord who demands tribute in the form of altered liver enzymes and contraindicated meds. The real virus was never in the blood. It was in the pharmacokinetics.
Jeff Moeller
November 22, 2025 AT 11:10Think about it. The body’s detox system is designed to clear toxins. Ritonavir turns that system into a hostage situation. CYP3A4 isn’t just blocked-it’s erased. And then you wonder why people on statins crash or why warfarin turns into a death sentence. It’s not a side effect. It’s the system screaming. We’re playing god with enzymes and pretending it’s medicine.
Herbert Scheffknecht
November 24, 2025 AT 11:10There’s a philosophical truth here. Ritonavir is the ultimate paradox: a drug that saves lives by breaking the body’s natural rules. We use it because it works, even though it makes everything else dangerous. It’s like using a chainsaw to fix a watch. The watch ticks, but you’ve destroyed the clockmaker’s workshop. And now everyone’s scared to wind their own watches. We’ve outsourced biology to a chemical tyrant and called it progress.
Jessica Engelhardt
November 24, 2025 AT 11:15So let me get this straight-Big Pharma invented a drug that makes every other drug unpredictable so they can sell more monitoring kits and lab tests? And now they’re pushing Paxlovid with the same shit? This isn’t medicine. It’s a profit loop disguised as science. You think they care if you bleed out from rivaroxaban? No. They care if you’re still buying their next prescription. The real pandemic is corporate greed wrapped in white coats.
Martin Rodrigue
November 26, 2025 AT 02:26While the pharmacological mechanisms described are indeed complex and well-documented, it is imperative to recognize that LPV/r remains a critical component of antiretroviral therapy in resource-limited settings. The cost differential between LPV/r and integrase inhibitors is not trivial, and in many low-income nations, this regimen represents the only viable option for sustained viral suppression. Dismissing its utility without acknowledging structural inequities in global health access is both academically and ethically unsound.
Sherri Naslund
November 27, 2025 AT 13:38lol they say ritonavir is dangerous but what about the fact that it was originally developed by some pharma lab that got bought by Pfizer? and now they're using it to sell paxlovid? and you think that's a coincidence? they knew this shit would be perfect for a pandemic. they planned it. the liver damage? the rebound? the birth control failure? all features. not bugs. they want you dependent. they want you scared. they want you coming back for more pills. this isn't science. it's control.
Ashley Miller
November 29, 2025 AT 12:02So you're telling me the same drug that’s supposed to save people from HIV is now the reason people die from heart meds and blood thinners? And you call this progress? What’s next? A pill that cures cancer but makes your kidneys explode? This isn’t medicine. It’s a magic trick where the rabbit is your liver and the hat is Big Pharma’s quarterly earnings report.
Lauren Hale
November 29, 2025 AT 21:01I’ve seen this play out in clinic after clinic. A patient on LPV/r comes in for a routine visit, starts taking OTC ibuprofen for a headache, and six weeks later has acute kidney injury. Not because ibuprofen is dangerous-but because ritonavir turned their kidneys into a minefield. That’s why we don’t just check meds-we check *everything*. Coffee, turmeric, St. John’s wort, even grapefruit juice. One tiny thing you think is harmless can blow up your whole treatment. I tell my patients: if you didn’t get it from your HIV doctor, assume it’s a grenade.
Greg Knight
November 30, 2025 AT 21:47Look, I get it-ritonavir is a beast. But here’s the thing: in places where people don’t have access to dolutegravir, LPV/r is the difference between life and death. I’ve had patients in rural clinics who’ve been on it for 15 years. They’re healthy. They’re employed. They’re raising kids. Yeah, they need more labs. Yeah, they can’t take certain meds. But they’re alive. That’s not a failure of medicine. That’s a triumph of adaptation. The real problem isn’t LPV/r. It’s the system that lets people go without better options.
rachna jafri
December 1, 2025 AT 10:37They say LPV/r is a workhorse but I say it’s a Trojan horse. The same people who told you it was safe for birth control are the ones who told you vaccines were dangerous. They’re the same pharma giants who buried the truth about opioids. Ritonavir’s not a drug-it’s a distraction. While you’re busy checking drug interactions, they’re busy pricing dolutegravir at $287 so you can’t switch. They don’t want you safe. They want you hooked on their expensive fix. And the worst part? You’re still thanking them for it.
darnell hunter
December 2, 2025 AT 16:38The assertion that ritonavir’s dual inhibitory/inductive properties render it inherently dangerous is empirically valid. However, the conflation of clinical utility with moral condemnation is a fallacy. The drug’s risk profile is well-characterized, and its continued use in resource-constrained settings is a rational, evidence-based decision, not a failure of ethics. To characterize its deployment as nefarious is to misunderstand the calculus of global public health.