When you walk into a pharmacy and pick up a bottle of blood pressure pills, you might not realize you’re holding a piece of global economic strategy. The little white pill labeled as a generic version of a brand-name drug isn’t just cheaper-it’s one of the few forces holding back runaway healthcare costs worldwide. In 2025, global healthcare spending is projected to hit $10.5 trillion, with prescription drugs alone accounting for over $1.6 trillion. Without generics, that number could easily be double.
Generics Are the Silent Shock Absorbers in Healthcare Economies
Imagine a car driving over potholes without suspension. That’s what healthcare systems look like without generic drugs. When a brand-name drug loses its patent, generics enter the market and often cut prices by 80-95%. In the United States, generic drugs made up 90% of all prescriptions filled in 2024, but they accounted for just 20% of total drug spending. That’s the power of competition.
In countries like Germany, India, and Brazil, generic substitution isn’t optional-it’s policy. Pharmacists can swap brand names for generics unless the doctor specifically says no. This isn’t just convenience; it’s fiscal survival. In 2022, the average person in a high-income country spent $380 per year on prescription drugs. Without generics, that number would likely be over $1,800.
Why the U.S. Still Pays More for Drugs-Even With Generics
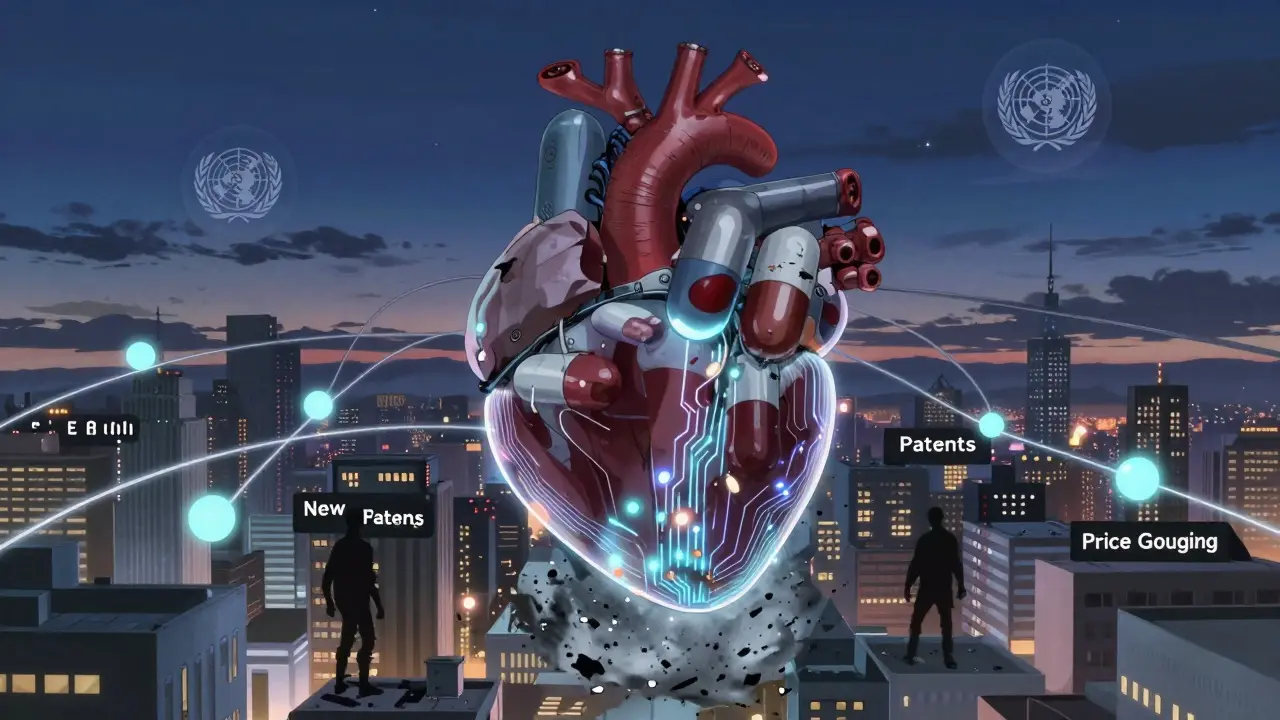
The U.S. spends more on prescription drugs than any other country. In 2025, it’s projected to spend $776 billion on prescriptions, up from $487 billion just one year earlier. That’s a 59% jump in a single year. Why? Because the biggest cost drivers aren’t the old, off-patent drugs-they’re the new ones.
Drugs for cancer, diabetes, obesity, and autoimmune diseases are getting more expensive. Many of these are biologics-complex molecules that can’t be easily copied. Even when biosimilars (the generic version of biologics) arrive, they face regulatory hurdles, slow adoption by doctors, and aggressive marketing from brand-name companies. As a result, only 15% of biologic spending in the U.S. is for biosimilars, even though they’re 15-35% cheaper.
Meanwhile, out-of-pocket costs for patients keep climbing. In 2025, the average American will pay $177 per person for prescriptions. By 2033, that’s expected to hit $231. That’s not inflation-it’s a tax on access. Generics help, but they can’t fix everything when the most expensive drugs are the ones with no generic alternatives.
Developing Countries Can’t Afford Innovation-So They Rely on Generics
In 55 countries, people pay for healthcare mostly out of their own pockets. In Turkmenistan, Afghanistan, and Nigeria, over 75% of healthcare costs come directly from households. There’s no insurance. No government subsidy. Just cash on the counter.
That’s why generics aren’t a preference-they’re the only option. In sub-Saharan Africa, 80-90% of all medicines are generics. In India, over 70% of the pharmaceutical market is made up of generic drugs produced domestically. These aren’t low-quality imports-they’re FDA- and WHO-approved versions of the same drugs sold in the U.S. and Europe, but sold for pennies.
When a child in Malawi needs antibiotics, the difference between a $2 generic and a $20 brand-name version means life or death. And when public health budgets shrink-like in Lebanon, where real healthcare spending dropped 71% between 2019 and 2021-generics are the only thing keeping clinics open.

The Global Divide: High-Income vs. Low-Income Spending
Not all countries spend the same on health. In 2022, high-income countries spent an average of 5.8% of their GDP on healthcare. Upper-middle-income countries spent 4%. Lower-middle-income countries? Just 2.4%. And low-income countries? A staggering 1.2%.
That’s not a coincidence. It’s a reflection of what’s affordable. Generics make the difference between having a functional health system and having none at all. In countries where the government can’t afford to buy expensive new drugs, generics are the backbone of public health programs.
But here’s the catch: as these countries grow wealthier, they start wanting the latest drugs. China, for example, is shifting from a generic-heavy market to one that’s adopting more innovative medicines. That’s good for patients-but bad for budgets. Without strong generic policies in place, these countries risk falling into the same trap as the U.S.: unsustainable drug prices.
Why Biosimilars Are the Next Frontier
Biologic drugs-like Humira, Enbrel, and Keytruda-are the most expensive medicines on the market. A single dose can cost over $10,000 a year. These aren’t chemical pills. They’re living molecules made from living cells. That’s why they’re hard to copy.
Biosimilars are the closest thing to generics for these drugs. They’re not exact copies, but they’re proven to work just as well. In Europe, biosimilars have cut costs by 30-70% in some cases. In the U.S., adoption is slower. Doctors are hesitant. Insurers don’t always push them. Patients don’t know they exist.
But the numbers are clear: if just half of all biologic prescriptions switched to biosimilars in the U.S., the healthcare system could save over $100 billion over the next decade. That’s enough to cover millions of insulin prescriptions, mental health treatments, and cancer therapies for people who can’t afford them now.
The Real Cost of Not Using Generics
Every time a patient skips a dose because they can’t afford the brand-name drug, the system pays more later. Emergency room visits. Hospitalizations. Lost productivity. Chronic disease worsens. The economic ripple effect is massive.
Insurers know this. In the WTW Global Medical Trends Survey, 67% of insurers expect healthcare demand to rise sharply over the next three years. Mental health services alone are projected to see costs jump by 15% or more per person. That’s why generics for antidepressants, antipsychotics, and anti-anxiety meds are more important than ever.
And yet, in many places, policy doesn’t match need. In the Middle East and Africa, medical costs are rising at 12.1% annually-the fastest growth rate in the world. Without stronger generic policies, those numbers will keep climbing.
What Needs to Change
Generics aren’t magic. They won’t fix broken health systems. But they’re the most effective tool we have to slow the tide of rising costs. Here’s what works:
- Automatic substitution laws-where pharmacists can swap generics unless the doctor says no-cut costs without sacrificing care.
- Fast-track approval for generics and biosimilars speeds up market entry and lowers prices faster.
- Public procurement-governments buying generics in bulk-drives down prices even further.
- Physician education-doctors need to know generics are just as safe and effective.
The U.S. could save $100 billion a year if it matched Europe’s biosimilar adoption rates. Low-income countries could prevent millions of deaths if they protected their generic supply chains from patent abuses and price gouging.
Generics aren’t the future of healthcare. They’re the present. And if we stop treating them as a backup option and start seeing them as essential infrastructure, we might actually make healthcare affordable for everyone.
Why are generic drugs so much cheaper than brand-name drugs?
Generic drugs cost less because they don’t need to repeat the expensive clinical trials that brand-name drugs do. The original manufacturer spent years and billions developing the drug and proving it works. Once the patent expires, other companies can make the same drug using the same formula. They only need to prove it’s bioequivalent-meaning it works the same way in the body. That cuts development costs by 90%, which translates directly to lower prices.
Are generic drugs as safe and effective as brand-name drugs?
Yes. In the U.S., the FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also meet the same strict manufacturing standards. Studies show generics work just as well in treating conditions like high blood pressure, diabetes, and depression. The only differences are in inactive ingredients-like fillers or dyes-which don’t affect how the drug works.
Why don’t all countries use generics as much as the U.S.?
Some countries lack the regulatory systems to approve generics quickly. Others have laws that prevent pharmacists from substituting generics without a doctor’s permission. In many low-income countries, the problem isn’t policy-it’s supply. There simply aren’t enough generic manufacturers to meet demand. And in some places, doctors and patients still believe brand-name drugs are better, even when evidence says otherwise.
What’s the difference between a generic and a biosimilar?
Generics are exact copies of small-molecule drugs-like pills for cholesterol or blood pressure. Biosimilars are similar, but not identical, copies of complex biologic drugs made from living cells-like insulin or cancer treatments. Because biologics are so complex, biosimilars can’t be exact replicas. But they’re proven to work the same way and are significantly cheaper. Biosimilars are still rare in many countries due to high approval costs and slow adoption by doctors.
How do generics affect global health equity?
Generics are the biggest equalizer in global health. In high-income countries, they make chronic disease management affordable. In low-income countries, they’re the only reason millions of people can access antibiotics, antivirals, and heart medications. Without generics, countries like Malawi or Nigeria couldn’t afford basic healthcare. They’re not just cost-savers-they’re life-savers.



wendy parrales fong
December 26, 2025 AT 11:24Generics are the unsung heroes of modern medicine. I never thought about how much they keep families from choosing between rent and insulin until my mom had to pick one. Now I get it.
Shreyash Gupta
December 26, 2025 AT 13:23India makes 60% of the world’s generics 🇮🇳💊. You think your $5 blood pressure pill is cheap? It’s because someone in Hyderabad made it for 20 cents. Big Pharma hates us for it.
Jeanette Jeffrey
December 27, 2025 AT 03:14Oh wow, another ‘generics are magical’ fairy tale. Let me guess-you also think vaccines are just sugar pills and climate change is a hoax? People who romanticize generics never had to deal with a bad batch that gave them diarrhea for a week.
david jackson
December 27, 2025 AT 12:09Okay, but let’s go deeper-why does the FDA even allow generics to exist? Because capitalism doesn’t care about health, it cares about profit margins. The entire system is built on patent cliffs and regulatory loopholes. Big Pharma spends $10 billion developing a drug, then spends $2 billion marketing it, and then when the patent expires, some factory in Goa makes it for $0.03 and sells it for $1. And suddenly, we’re supposed to be grateful? No. We’re supposed to be furious. This isn’t innovation-it’s exploitation dressed up as affordability. The real scandal isn’t that generics exist-it’s that we let them be the only option for people who can’t afford the original. We’ve turned healthcare into a lottery where your life depends on whether your insurance covers the generic version of a drug that was originally priced at $10,000 a pill. And we call this progress?
carissa projo
December 28, 2025 AT 18:28Generics don’t just save money-they save dignity. I’ve seen grandparents skip doses because they couldn’t afford the brand, then end up in the ER three months later. That’s not a medical failure. That’s a moral one. The fact that we’ve normalized this is terrifying. Imagine if we treated food the same way-‘Oh, you can’t afford the organic kale? Here’s some expired cabbage.’ We’d be outraged. But when it’s medicine? We shrug. Maybe we need to start calling these drugs what they really are: lifelines, not line items.
josue robert figueroa salazar
December 30, 2025 AT 03:08Generics are fine. Until they’re not. Seen too many people get sick because the filler in the generic made them break out. Don’t romanticize it.
Angela Spagnolo
December 31, 2025 AT 14:39...I just... I mean... generics... they're... important... right? I think? I read somewhere... yeah... I guess...?
Michael Bond
January 2, 2026 AT 03:03Biosimilars need faster approval. That’s it.
Matthew Ingersoll
January 2, 2026 AT 04:52India’s generic industry is one of the most underrated global contributions. The WHO relies on Indian generics for 80% of its HIV and malaria meds. This isn’t just commerce-it’s global public health infrastructure. And yet, we treat it like a discount aisle.
christian ebongue
January 3, 2026 AT 10:18Oh cool, so now generics are saving the world? Meanwhile, my insurance raised my copay on the generic version by 40% last year. Thanks, capitalism.
Ryan Cheng
January 3, 2026 AT 13:22Shreyash’s point about India is spot on. I worked with a pharma startup in Hyderabad last year-those labs are insane. Precision, scale, ethics. And they’re not cutting corners. The FDA inspects them more than some U.S. plants. The real problem isn’t quality-it’s perception. People still think ‘generic’ means ‘cheap knockoff.’ It’s time we rebranded it as ‘equitable science.’
Jody Kennedy
January 4, 2026 AT 14:59Let’s not forget: generics are how we get antivirals to kids in Malawi. That $2 pill? It’s not just a drug. It’s a chance. And if we let patent trolls and lobbying kill that, we’re not just failing the economy-we’re failing humanity.