When you're an athlete, your hips don't just move-they power every sprint, twist, jump, and kick. But if you've been feeling deep groin pain, clicking, or stiffness that won't go away, you might be dealing with something more serious than a strain: a hip labral tear. This isn't just a minor injury. For athletes under 40, especially in sports like soccer, basketball, hockey, and ballet, it's one of the most common causes of persistent hip pain. And if it's not caught early, it can lead to early arthritis.
What Exactly Is a Hip Labral Tear?
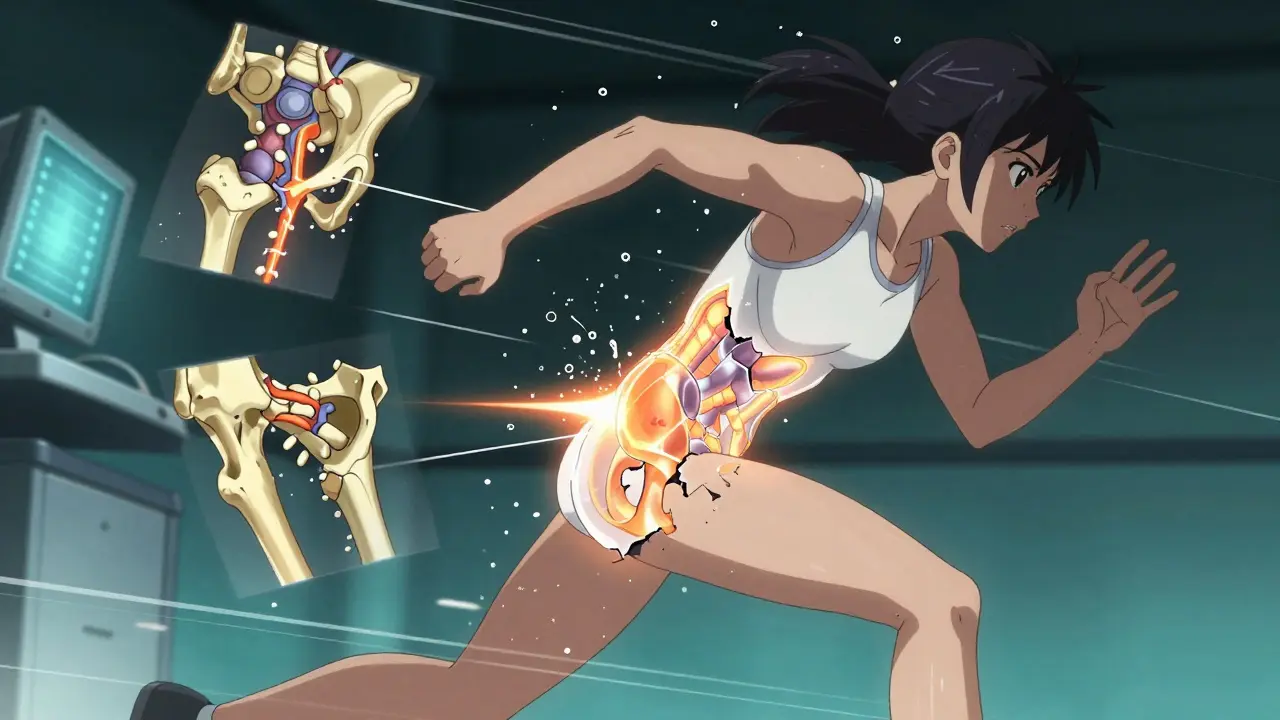
The labrum is a ring of tough, rubbery cartilage that wraps around the socket of your hip joint. Think of it like a gasket that seals the ball-and-socket joint, keeping everything stable and cushioned. When it tears, you don't just feel pain-you lose stability. The labrum helps hold the femoral head in place, and when it's damaged, the joint doesn't glide smoothly anymore. That’s when you get catching, locking, or that annoying click you can't ignore. Most tears happen because of repetitive stress or structural problems. The biggest culprit? Femoroacetabular impingement (FAI). This is when the bones of your hip aren't shaped right-either the ball is too bumpy or the socket is too shallow-and they rub against each other over time. It’s like a misaligned gear grinding itself down. About 70% of labral tears in athletes are linked to FAI, according to Cleveland Clinic data from 2023.Who’s Most at Risk?
It’s not just professional athletes. College players, elite dancers, and even serious weekend warriors are getting diagnosed more than ever. Sports that demand deep hip rotation-like soccer, hockey, gymnastics, and long-distance running-put the most strain on the labrum. A 2022 study in the American Journal of Sports Medicine found that basketball players account for 22% of cases, soccer for 18%, and hockey for 15%. Runners aren’t off the hook either-12% of labral tears occur in them. Age matters too. Most patients are under 40. Why? Because older hips tend to show signs of arthritis, which masks the labral tear. In younger athletes, the tear is often the main problem. But if you're over 35, your chances of returning to the same level of play drop to 70-75%, compared to 85-90% for younger athletes, according to Cleveland Clinic.How Do You Know It’s a Labral Tear?
Pain in the front of the hip or groin is the big red flag. But it’s not always obvious. Many athletes think it’s a pulled muscle or a hip flexor strain and wait weeks-or months-to get checked. That’s a mistake. The longer you wait, the more damage can happen. Doctors use two key physical tests to spot it:- FADIR test: Flex your hip, pull your knee toward your chest, then rotate it inward. If this causes sharp pain, it’s a strong indicator.
- FABER test: Lie on your back, bend your knee, and place your ankle on the opposite knee. Press down gently. Pain or a click here can point to a labral issue.
Imaging: The Right Tests for the Right Diagnosis
You might think an MRI is enough. But standard MRI misses up to 30% of labral tears, especially partial ones. That’s why the gold standard for imaging is magnetic resonance arthrography (MRA). MRA involves injecting contrast dye into the hip joint before the scan. This dye highlights the labrum, making even tiny tears visible. Studies show MRA has 90-95% sensitivity and 85-92% specificity. The International Hip Documentation Society recommends it for preoperative planning because it can detect tears as small as 0.1-0.2mm. X-rays come first-not to see the tear, but to spot underlying problems. Doctors look for hip dysplasia (a shallow socket), bone spurs, or signs of arthritis. If the X-ray shows a shallow socket, that changes everything. Repairing the labrum alone in a dysplastic hip leads to a 60-70% re-tear rate. You need to fix the bone structure too. And here’s the catch: many athletes hit insurance roadblocks. A standard MRI costs $500-$800. MRA? $1,200-$1,800. A 2023 Healthgrades survey found 68% of patients had to pay out-of-pocket for MRA. That delay can cost you months of recovery time.
Conservative Treatment: Can You Avoid Surgery?
Not everyone needs surgery. About 30-40% of athletes see no improvement with rest and PT, but True Sports Physical Therapy reports that 65% of patients manage symptoms without surgery-especially if they’re not in high-impact sports. The first step? Rest. Stop the sport that hurts. Use NSAIDs like ibuprofen or naproxen to reduce inflammation. Then, physical therapy focused on hip stability and core strength. But here’s the problem: general PT doesn’t cut it. You need a therapist who understands hip biomechanics. They’ll work on:- Strengthening the gluteus medius to stabilize the pelvis
- Improving hip internal rotation without pain
- Correcting movement patterns that caused the tear
Arthroscopy: The Gold Standard
If conservative treatment fails, hip arthroscopy is the next move. It’s minimally invasive, done through two or three small incisions. A tiny camera goes in, and the surgeon can see the labrum directly-98% diagnostic accuracy, according to Cleveland Clinic. There are two main procedures:- Debridement: Trimming away the torn, frayed part of the labrum. Faster recovery-3-4 months to return to sport.
- Repair: Sewing the labrum back to the bone using suture anchors. Takes longer-5-6 months-but preserves the natural structure.
Recovery: It’s Not Just About Time
Recovery isn’t just waiting for pain to go away. It’s rebuilding strength and movement safely. A typical rehab plan has four phases:- Protection (weeks 1-6): No weight-bearing on the hip, no twisting. Use crutches if needed.
- Strengthening (weeks 7-12): Focus on glutes, quads, core. Goal: 90% strength symmetry between legs.
- Sport-specific training (weeks 13-20): Agility drills, controlled pivoting, jumping.
- Return to sport (weeks 21-26): Only when you can rotate your hip to 30 degrees internally without pain.
What About Underlying Issues?
This is where most treatment plans fail. If you have hip dysplasia, FAI, or acetabular retroversion, fixing the labrum alone is like patching a leaky roof without fixing the foundation. Dr. Andrea Stracciolini of Boston Children’s Hospital says: “If they have hip dysplasia and a labral tear, we talk about most likely needing to fix the dysplasia surgically.” The American Academy of Orthopaedic Surgeons (AAOS) warns that isolated labral debridement without correcting structural issues leads to 40% higher revision rates. That’s why top sports centers now use 3D MRI sequencing for complex cases-improving accuracy to 97% as shown in a May 2023 study.Complications and Long-Term Risks
Hip arthroscopy is safe, but not risk-free. About 15-20% of patients still have persistent pain. Heterotopic ossification (bone growing where it shouldn’t) happens in 5-10% of cases. Nerve injury is rare-1-2%-but can cause numbness. The biggest long-term risk? Osteoarthritis. A 15-year study in the Journal of Bone and Joint Surgery found untreated labral tears increase the risk of hip OA by 4.5 times within a decade. That’s why early, accurate diagnosis and proper treatment aren’t just about getting back to the field-they’re about protecting your hip for life.Real Stories, Real Outcomes
On Reddit, u/TrackDoc2020, a marathon runner, returned to training at 4.5 months after repair with 12 weeks of targeted PT. But another athlete, a dancer, kept hearing clicks and needed revision surgery because the first diagnosis missed the full extent of the tear. NHL player Ryan Nugent-Hopkins took 5.5 months to return to pro hockey after his repair. That’s typical for high-demand sports. Athletes who go to specialized sports medicine centers report 92% satisfaction. Those treated at general orthopedic clinics? Only 75%. The difference? Expertise in hip biomechanics, access to MRA, and tailored rehab.What’s Next for Hip Labral Care?
The field is moving fast. Regenerative medicine like PRP (platelet-rich plasma) injections is showing promise-55% of patients in a 2022 HSS trial avoided surgery at 12 months. But it’s not a magic fix. It works best for small tears or as a bridge to surgery. By 2027, experts predict 75% of labral repairs will be done with all-arthroscopic techniques, up from 60% today. The market for hip arthroscopy is growing at 12.3% a year and hit $1.2 billion in 2022. More athletes are getting diagnosed. More surgeons are trained. More tools are available. But the core hasn’t changed: early detection, accurate imaging, and addressing root causes are what make the difference between a comeback and a career-ending injury.Can a hip labral tear heal on its own?
No, the labrum has very little blood supply, so it can’t heal by itself. Minor tears might become less painful with rest and physical therapy, but the tear itself won’t close. Without treatment, the damage can worsen, leading to joint instability and early arthritis.
Is MRA always necessary for diagnosis?
Not always, but it’s strongly recommended for athletes. Standard MRI misses up to 30% of labral tears, especially partial ones. If you’re an athlete with persistent hip pain and normal X-rays, MRA is the best way to confirm the diagnosis before deciding on surgery. Insurance may be a barrier, but skipping it can lead to misdiagnosis and failed treatment.
How long does it take to return to sports after hip arthroscopy?
It depends on the procedure. Debridement usually allows return in 3-4 months. Labral repair takes longer-5-6 months. But timing isn’t just about weeks. You must hit strength and mobility milestones: 90% quadriceps symmetry, pain-free hip internal rotation to 30 degrees, and no swelling during activity. Rushing back increases re-injury risk.
Can you prevent a hip labral tear?
You can’t always prevent it, especially if you have anatomical issues like FAI or dysplasia. But you can reduce risk by strengthening hip stabilizers (glutes, core), avoiding overtraining, correcting movement patterns, and getting checked if you have persistent groin pain. Early detection is the best prevention.
Does surgery guarantee a return to sport?
No, but it gives you the best chance. About 85-90% of athletes under 40 return to their previous level after arthroscopy, especially when structural issues are fixed. But success depends on the surgeon’s skill, rehab adherence, and whether underlying problems like hip dysplasia were addressed. Athletes over 35 have lower return rates, and those in high-impact sports like hockey or ballet face higher complication risks.


Tiffany Adjei - Opong
January 6, 2026 AT 14:59Okay but have you actually looked at the insurance data? Most people can't even get MRA approved-so they get misdiagnosed with 'hip flexor strain' and end up with a full tear by the time they finally see a specialist. And then they blame the surgeon when it doesn't work. It's not the surgery-it's the system.
Ryan Barr
January 6, 2026 AT 23:08MRA is overkill. Most tears are degenerative. Stop overmedicalizing athletes.
Cam Jane
January 8, 2026 AT 07:39Y’all need to hear this: if you’re an athlete with hip pain and your PT is just doing squats and foam rolling, you’re being set up to fail. I’ve seen 17-year-old dancers come in with labral tears and their coaches say ‘just stretch more.’ NO. You need biomechanics. You need glute medius activation drills. You need gait analysis. You need someone who’s actually studied hip kinematics-not just a general PT who does ‘core work’ on a BOSU ball. I had a client who missed her NCAA qualifiers because she waited 11 months to get MRA. Now she’s back on the floor, pain-free, after repair + 6 months of targeted rehab. Don’t wait. Get the right scan. Find the right expert. Your hip doesn’t have time for guesswork.
Tom Swinton
January 9, 2026 AT 18:07I just want to say-I was that guy. 28, college basketball, thought it was just tight hips. Took 8 months to get an MRA because my insurance kept denying it. I cried in the waiting room when the radiologist pointed out the tear on the screen. I didn’t even know what a labrum was. But after surgery, after the 6-month rehab where I had to relearn how to walk without limping-I got my life back. Not just my game. My sleep. My mood. My confidence. Don’t ignore the click. Don’t wait for it to ‘warm up.’ Get it checked. You’re not weak for needing help. You’re smart for asking.
Katelyn Slack
January 11, 2026 AT 00:45what if you cant afford mra?? like im a student and my insurance only covers mri and i have the pain but no money for extra tests??
Melanie Clark
January 12, 2026 AT 06:55This is all just a pharmaceutical-industrial complex ploy to sell more MRIs and surgeries. The body heals itself if you stop overloading it. You don’t need a camera in your hip. You need less sugar, more sleep, and to stop pretending you’re a professional athlete because you play pickup basketball once a week. The real epidemic is overtraining and poor nutrition-not labral tears. And don’t get me started on PRP. It’s snake oil with a fancy name.
Harshit Kansal
January 13, 2026 AT 19:46Bro I had this exact thing last year. Played football in college. Thought it was just a groin pull. Went to a regular ortho. They said rest. I rested. Three months later I could barely walk. Got a second opinion. MRA showed full tear. Surgery. 5 months later back on the field. But man-don’t skip the MRA. It’s worth every penny.
Venkataramanan Viswanathan
January 14, 2026 AT 07:52In India, access to MRA is nearly impossible outside major cities. Most athletes here are diagnosed via clinical examination alone. We rely on FADIR and FABER tests with ultrasound as a supplement. The success rate is lower, but we adapt. The real issue is not the technology-it is the lack of awareness among coaches and parents. A 16-year-old sprinter with chronic groin pain is often told to 'run through it.' We need grassroots education, not just high-tech imaging.
Kiran Plaha
January 14, 2026 AT 09:23so if you have faI and labral tear, you need bone surgery too? like osteotomy? that sounds scary. is it common?
Matt Beck
January 15, 2026 AT 20:10It’s not just a tear… it’s a metaphysical rupture. The labrum? It’s the soul of your hip’s architecture. When it fails, you’re not just losing cartilage-you’re losing alignment with the universe’s natural motion. We treat the body like a machine, but it’s a symphony. And when one note is off… the whole piece collapses. PRP? Maybe it’s not about healing tissue… maybe it’s about restoring harmony. 🌌
Molly McLane
January 15, 2026 AT 23:00Hey-this is such an important post. If you’re reading this and you’re scared to ask for help, please know: you’re not alone. I’ve coached high school athletes for 12 years and I’ve seen too many kids push through pain until they’re sidelined for a year. Talk to your coach. Ask for a referral. Get the MRA. It’s not a luxury-it’s an investment in your future self. And if you’re a parent, don’t dismiss your kid’s pain as ‘growing pains.’ It’s not. Be their advocate. You’ve got this.