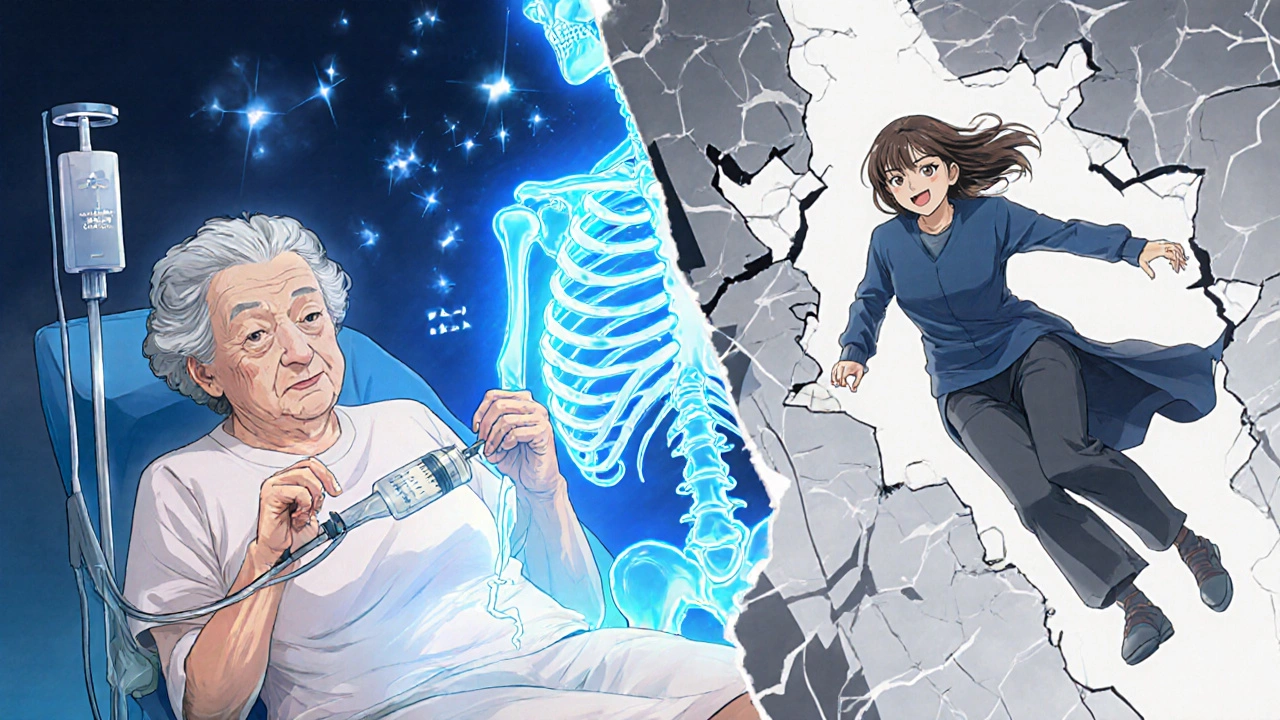
Breaking a bone isn’t just painful-it can change your life. For people over 50, a hip fracture often means losing independence. About 1 in 3 women and 1 in 5 men over 50 will suffer an osteoporosis-related fracture in their lifetime. The good news? Many of these fractures are preventable. But not all supplements and medications work the same way. And some that seem harmless might not help at all-or could even hurt.
Calcium and Vitamin D: The Basics That Don’t Always Work
You’ve heard it a thousand times: “Take calcium and vitamin D for strong bones.” But here’s the truth: taking low doses of both doesn’t reduce your risk of breaking a bone. The U.S. Preventive Services Task Force found that if you’re taking 400 IU of vitamin D or less than 1,000 mg of calcium daily, you’re not getting any real protection. That’s because your body needs enough of both to even start building bone.
Here’s what actually works: 800-1,000 IU of vitamin D3 plus 1,000-1,200 mg of calcium per day. That combination, shown in multiple large studies, reduces hip fractures by about 16% and any fracture by 6%. But only if you’re deficient. If your vitamin D level is already above 20 ng/mL, adding more won’t help. And if you’re eating enough calcium through food-dairy, leafy greens, fortified foods-you probably don’t need pills.
The problem? Most people think vitamin D is a magic bullet. A 2022 study found that 35% of U.S. adults over 50 take vitamin D supplements, and nearly 1 in 5 are taking more than the safe upper limit of 4,000 IU daily. That’s not just useless-it’s risky. High doses of calcium (over 1,000 mg/day from supplements) are linked to a 17% higher chance of kidney stones and even a small increase in heart problems.
Who Actually Benefits from Supplements?
Not everyone. Supplements only make a real difference for people who are truly deficient or at high risk:
- People living in nursing homes or care facilities (they rarely get sunlight or eat enough calcium)
- Those with a blood vitamin D level below 20 ng/mL
- People who eat less than 700 mg of calcium daily
- Older adults who’ve already had a fracture
For example, the famous 1992 Chapuy study showed a 43% drop in hip fractures among nursing home residents given 800 IU vitamin D and 1,200 mg calcium. But when the same doses were tested on healthy, active older adults living at home-people with vitamin D levels around 18.5 ng/mL-the results were zero. No benefit. That’s why doctors now test your vitamin D level before prescribing supplements. It’s not guesswork anymore.
Bone-Building Medications: When Supplements Aren’t Enough
If you’ve already broken a bone, or your FRAX® score says you have a 20% or higher chance of breaking one in the next 10 years, supplements alone won’t cut it. You need stronger tools. These are the five main classes of bone-building medications:
- Bisphosphonates (alendronate, risedronate, zoledronic acid): These slow bone loss. Alendronate cuts vertebral fractures by 44%. Zoledronic acid (given as a yearly IV) reduces hip fractures by 41% over 18 months.
- Denosumab (Prolia): A monthly or twice-yearly injection that blocks bone breakdown. Reduces spine fractures by 68% and hip fractures by 40%.
- Teriparatide (Forteo) and Abaloparatide (Tymlos): These are anabolic drugs-they actually build new bone. Teriparatide reduces spine fractures by 65% and is now approved for men too.
- Romosozumab (Evenity): A newer drug that builds bone while slowing loss. Reduces spine fractures by 73% in the first year.
These aren’t mild treatments. They’re powerful. That’s why doctors don’t hand them out like aspirin. You need a bone density scan (DXA), a FRAX® score, and often blood tests before starting. And you need to stick with them. Half of people stop taking bisphosphonates within a year because of stomach upset or fear of rare side effects.
The Hidden Risks: What No One Tells You
Every medication has trade-offs. Bisphosphonates carry a tiny risk of jawbone death (osteonecrosis)-about 1 in 10,000 patients after 5 years. Atypical femur fractures are even rarer, but they happen. That’s why dentists now ask about your bone meds before pulling teeth. And if you’ve been on a bisphosphonate for more than 5 years, your doctor might suggest a “drug holiday” to lower risk.
Denosumab works great-but if you stop it suddenly, you can lose bone fast. That’s why you can’t just quit. You need to switch to another medication right away.
Teriparatide and abaloparatide are limited to 2 years of use because long-term safety isn’t fully known. After that, you usually move to a bisphosphonate or denosumab to hold onto the new bone you built.
And yes, calcium supplements can cause constipation. Many people quit because of it. If that’s you, try calcium citrate instead of calcium carbonate. It’s gentler on the stomach and absorbs better without food.
How to Know What You Need
Here’s the step-by-step path most doctors follow:
- Get a FRAX® score-it’s free online and calculates your 10-year fracture risk based on age, sex, weight, past fractures, and other factors.
- Get a bone density scan (DXA) if your FRAX® score is borderline or you’ve had a fracture.
- Test your vitamin D level (25-hydroxyvitamin D). If it’s below 20 ng/mL, you need correction.
- If you’re deficient in vitamin D, start with high-dose therapy: 50,000 IU of vitamin D2 once a week for 8-12 weeks, then switch to 800-2,000 IU daily.
- Check your calcium intake. If you’re eating less than 700 mg/day from food, add a supplement to hit 1,000-1,200 mg total.
- If your fracture risk is high (FRAX® >20%), talk to your doctor about bone-building meds. Don’t wait until you break another bone.
Don’t rely on online quizzes or pharmacy recommendations. These tools are designed to sell pills, not prevent fractures. Real prevention is personalized.
What’s New in 2025?
The field is moving fast. In 2023, the FDA approved abaloparatide for men with osteoporosis-finally giving men the same powerful bone-building options as women. The European Society for Clinical and Economic Aspects of Osteoporosis now recommends starting with anabolic drugs (like teriparatide) for people with severe bone loss, then switching to antiresorptives. This “sequential therapy” cuts new spine fractures by 73% more than bisphosphonates alone.
The VITAL-DEP trial, still running, is testing whether high-dose vitamin D (2,000 IU/day) helps older adults with depression and low vitamin D levels prevent fractures. Results are due by late 2025. Early data suggests depression and low vitamin D often go hand-in-hand-and both raise fracture risk.
Meanwhile, the market is booming. Osteoporosis drugs hit $10.7 billion in sales in 2022, and that’s expected to grow to $14.3 billion by 2028. But here’s the irony: even with all this innovation, more than half of people stop their meds within a year. Why? Side effects, cost, forgetfulness, or just not understanding how serious the risk is.
Bottom Line: What to Do Right Now
If you’re over 50 and haven’t broken a bone:
- Don’t take low-dose vitamin D and calcium pills unless your doctor says so.
- Get your vitamin D level checked. If it’s low, fix it properly.
- Eat more calcium-rich foods: yogurt, cheese, sardines, kale, fortified plant milks.
- Walk 30 minutes a day. Weight-bearing exercise builds bone better than any pill.
If you’ve already broken a bone, or your doctor says you have osteoporosis:
- Don’t delay treatment. Every month without treatment increases your risk of another fracture.
- Ask for a FRAX® score and DXA scan if you haven’t had them.
- Discuss all options-not just the cheapest or most advertised drug.
- Stick with your treatment. The best drug is the one you take.
Fracture prevention isn’t about popping a daily pill. It’s about knowing your risk, testing your levels, and choosing the right tools-whether that’s food, sunlight, exercise, or medicine. The science is clear. Now it’s up to you to act on it.


Manish Pandya
November 26, 2025 AT 02:30Finally, someone cuts through the supplement hype. I’ve seen so many older folks take calcium pills and call it a day-then end up in the ER after a simple slip. The 16% fracture reduction stat with proper dosing? That’s the real deal. And yeah, most people don’t need pills if they’re eating yogurt, sardines, and kale. My aunt took 2,000 mg of calcium daily for years-ended up with kidney stones. She didn’t even know.
Terry Bell
November 26, 2025 AT 05:37Man, this hit different. I used to think vitamin D was like a multivitamin-more is better, right? Nope. Turned out my levels were fine, I was just taking it because ‘everyone does.’ Now I get outside for 20 mins a day, eat cheese, and walk my dog. No pills. My bones feel stronger, and my wallet’s happier. Life’s too short for unnecessary supplements. 🌞💪
Lawrence Zawahri
November 26, 2025 AT 12:19THEY DON’T WANT YOU TO KNOW THIS. The pharmaceutical industry is pushing these meds because they make BILLIONS. Vitamin D? They say it’s useless unless you’re deficient-but what if they’re lying about what ‘deficient’ even means? And why do they only test D levels if you’re over 50? Coincidence? I think not. The ‘drug holiday’? That’s just a trick to get you back on the cycle. Wake up people. 💉👁️
Rachelle Baxter
November 27, 2025 AT 16:37OMG. I’m so glad this was posted. I’ve been telling my mom for YEARS that she doesn’t need that 2,000 IU vitamin D pill she takes every morning. She’s healthy, eats dairy, gets sunlight. And now science backs me up! 🙌 Also, calcium carbonate causes constipation? No wonder she’s always grumpy. Switched her to citrate-she’s pooping like a champ now. 😅
Dirk Bradley
November 28, 2025 AT 04:42It is both intellectually and ethically imperative to recognize that the current paradigm of osteoporotic prophylaxis is fundamentally misaligned with the empirical evidence base. The indiscriminate supplementation of calcium and vitamin D constitutes a paradigmatic example of evidence-ignoring populism in clinical practice. One must consult the U.S. Preventive Services Task Force guidelines-not the wellness influencer on Instagram.
Emma Hanna
November 29, 2025 AT 13:03Wait-so you’re telling me that taking a $20 bottle of calcium from Walmart isn’t enough? That’s insane. I’ve been doing it for 10 years. My mom broke her hip at 78, and I thought I was being proactive. But now I realize… I was just wasting money. And my doctor never even tested my vitamin D. Why not?!!??
Mariam Kamish
November 30, 2025 AT 10:49Ugh. Another ‘science’ article that sounds smart but ignores real life. Who has time to get a DXA scan? Or a FRAX score? My insurance won’t cover it. And I work two jobs. I just want to live without breaking a bone. So yeah, I’ll keep taking my cheap pills. At least they make me feel like I’m doing something.
🤷♀️Patrick Goodall
December 1, 2025 AT 09:55They say ‘don’t wait until you break another bone’ but what if you already broke three? And the meds made you feel like a zombie? And your doctor just shrugs and says ‘try the next one’? I’m 62 and I’ve been on four different drugs. Now they want me to switch to Evenity? That’s $30K a year. And I’m on Medicare. This ain’t medicine. This is a pyramid scheme with IV drips.
💸😭Adesokan Ayodeji
December 1, 2025 AT 19:25Bro, I’m from Nigeria and we don’t have access to all this fancy testing, but we know one thing: if you’re eating yam, beans, leafy greens, and walking every day, you’re already ahead. My uncle, 72, never took a supplement, but he carries his grandkids on his back every Sunday. No fractures. No meds. Just movement and real food. The science here is solid, but don’t forget the power of simple living. Your bones aren’t made in a lab-they’re built by walking, eating, and staying active. You don’t need a prescription to be strong.
Karen Ryan
December 2, 2025 AT 16:06As someone who moved from Japan to the U.S., I’ve seen how different cultures approach this. In Japan, they eat fish, tofu, seaweed, and green tea-high in calcium and antioxidants. No pills. No scans. Just daily habits. And their fracture rates are lower than ours. Maybe we’re overcomplicating this. The answer isn’t always a drug-it’s food, sun, and movement. Simple. But hard to do in a fast-paced life.
🌏🥢