Fluocinolone Safety Calculator
Fluocinolone Usage Risk Assessment
This tool estimates your risk of side effects based on your usage pattern. Remember: short-term, limited use is safer than prolonged application.
Risk Assessment Results
Key Side Effects to Monitor
Safety Recommendations
When you hear the name fluocinolone, you probably picture a cream that eases itching and redness. What most people don’t realize is that this tiny molecule is a powerful player in the body’s immune orchestra. Below we break down how fluocinolone talks to immune cells, why doctors harness it for skin disorders, and what hidden risks you should keep an eye on.
What Is Fluocinolone?
Fluocinolone is a synthetic corticosteroid designed for topical use. First synthesized in the 1970s, it belongs to the class of medium‑potency glucocorticoids and is marketed under brand names like Florone and Synalar. Its chemical structure adds a fluorine atom to the steroid backbone, which boosts anti‑inflammatory power while keeping skin penetration relatively low.
How Fluocinolone Talks to the Immune System
All corticosteroids share a common route: they slip into cells, bind the glucocorticoid receptor (GR), and travel to the nucleus. Once there, the receptor‑ligand complex flips on genes that produce anti‑inflammatory proteins (like annexin‑1) and flips off genes that make pro‑inflammatory cytokines (such as IL‑1, IL‑6, and TNF‑α). Fluocinolone is no exception, but its fluorine tweak gives it a tighter grip on the GR, which translates into a stronger, quicker shutdown of the immune response.
Key immune cells affected include:
- T‑lymphocytes: Their activation and proliferation drop sharply, reducing the cascade that leads to skin lesions.
- Macrophages: Production of nitric oxide and reactive oxygen species is dampened, easing tissue damage.
- Dendritic cells: Antigen presentation slows, meaning the skin sees fewer “danger” signals.
The net effect is less swelling, fewer red patches, and a calmer itch reflex.
Clinical Uses: When Doctors Choose Fluocinolone
Because it hits the immune system without roving the whole body, fluocinolone shines in several dermatologic conditions:
- Atopic dermatitis: Chronic eczema sufferers get a noticeable itch reduction after just a few days.
- Psoriasis: Though not as potent as clobetasol, fluocinolone can tame mild plaques on the elbows and knees.
- Lichen planus: The drug eases the violaceous, flat‑topped bumps that often bother mucosal surfaces.
- Contact dermatitis: When an irritant or allergen triggers a rash, a short course of fluocinolone speeds up recovery.
In each case, the goal is to curb the local immune overdrive while sparing the rest of the body from systemic side effects.
Potential Risks and How to Monitor Them
Even a topical steroid can tip the balance if used improperly. The main hazards revolve around too‑much immunosuppression and skin barrier damage.
| Risk | What Happens | How to Spot It |
|---|---|---|
| Skin thinning (atrophy) | Collagen breakdown in the dermis | Visible translucency, easy bruising |
| Telangiectasia | Dilated superficial blood vessels | Red spider‑like lines on the surface |
| Local infection | Immune suppression allows microbes to flourish | Increased redness, pus, foul odor |
| Systemic absorption | Part of the drug enters bloodstream | Adrenal suppression symptoms: fatigue, dizziness |
Guidelines to keep risk low:
- Apply a thin layer once or twice daily-never more.
- Limit continuous use to two‑week intervals, then give the skin a break.
- Avoid covering the area with occlusive dressings unless prescribed.
- Watch for signs of adrenal suppression, especially in children or when large body surface areas are treated.
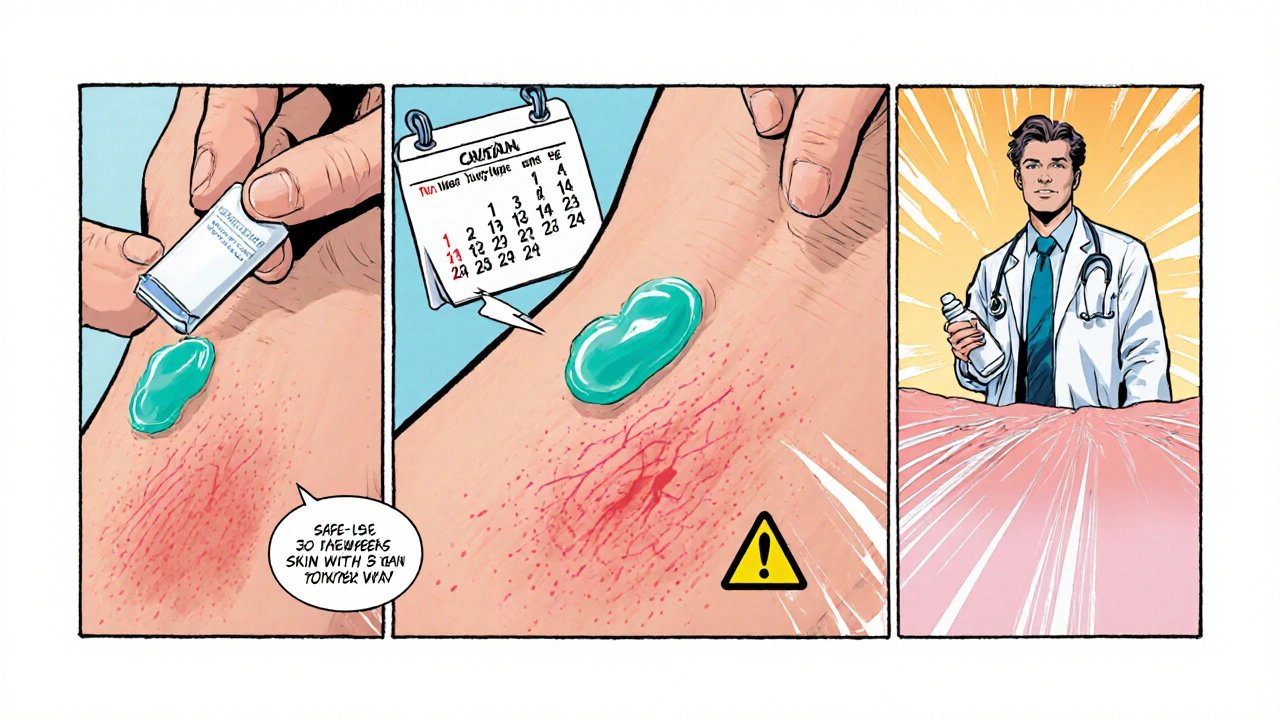
Patient Tips: Getting the Most Out of Fluocinolone
Think of fluocinolone as a short‑term ally, not a permanent fix. Here are practical steps that help you stay safe and see results faster:
- Clean, dry skin first: Moisture barriers keep the drug from slipping off.
- Use a fingertip unit: One fingertip‑sized amount treats roughly a palm‑sized area.
- Combine with moisturizers: After the steroid dries, lock in moisture with a fragrance‑free emollient to restore barrier function.
- Track progress: Jot down itch intensity and redness each day; if no improvement after 5‑7 days, contact your clinician.
- Know the exit plan: Your doctor may taper the dose or switch to a milder steroid to prevent rebound flare‑ups.
Frequently Asked Questions
Can fluocinolone be used on the face?
Yes, but only for short periods and under a doctor’s supervision. The facial skin is thin, so the risk of atrophy or acne‑like eruptions is higher.
Is fluocinolone safe for children?
It can be prescribed for kids with atopic dermatitis, but the dose is lower and treatment duration is tightly limited to avoid adrenal suppression.
How does fluocinolone differ from clobetasol?
Clobetasol is a super‑potent steroid used for severe plaques; fluocinolone sits in the medium‑potency range, offering a better safety profile for everyday use on sensitive areas.
Can I apply fluocinolone over an infection?
No. Applying a steroid on an active bacterial, fungal, or viral infection can make the infection worse by dampening the local immune response.
What should I do if I miss a dose?
Just apply it as soon as you remember, then continue with the regular schedule. Don’t double‑dose to catch up.
Is there a risk of systemic side effects?
Systemic effects are rare with proper use, but large‑area or prolonged application can suppress the hypothalamic‑pituitary‑adrenal axis, leading to fatigue, low blood pressure, or trouble handling stress.
How long does it take to see improvement?
Most patients notice reduced redness and itching within 3‑5 days. Full lesion flattening may take 1‑2 weeks.



John Magnus
October 16, 2025 AT 16:14Fluocinolone exemplifies the intricate pharmacodynamics of medium‑potency glucocorticoids, as its fluorinated scaffold confers a heightened affinity for the glucocorticoid receptor, thereby amplifying transcriptional repression of NF‑κB‑mediated cytokine cascades. The ligand‑receptor complex translocates to the nucleus, where it recruits co‑repressors and histone deacetylases, resulting in epigenetic silencing of pro‑inflammatory genes such as IL‑1β, IL‑6, and TNF‑α. Simultaneously, it induces annexin‑1 expression, a pivotal anti‑inflammatory mediator that attenuates phospholipase A2 activity and curtails arachidonic acid metabolites. This dual mechanism underlies the rapid abatement of erythema and pruritus observed in atopic dermatitis, psoriasis, and lichen planus. Moreover, the drug’s limited percutaneous absorption mitigates systemic cortisol suppression, preserving hypothalamic‑pituitary‑adrenal axis integrity when applied judiciously. However, the pharmacokinetic profile is not uniform; occlusive dressings or extensive body‑surface coverage can surge systemic bioavailability, precipitating iatrogenic adrenal insufficiency. Dermatologists must therefore balance potency against barrier integrity, employing the fingertip unit method to quantify dosage precisely. The dermal extracellular matrix benefits from intermittent steroid holidays, which allow fibroblast collagen synthesis to rebound, averting atrophic sequelae. In pediatric cohorts, the risk‑benefit calculus skews toward minimizing exposure duration, given the heightened susceptibility of developing adrenal glands. From an immunological standpoint, fluocinolone dampens dendritic cell maturation, curtailing antigen presentation and T‑cell priming-a double‑edged sword that can impede host defense against cutaneous pathogens. Consequently, clinicians should co‑prescribe emollients to restore barrier function and monitor for secondary infections. The overarching therapeutic paradigm hinges on short‑term, high‑impact intervention followed by maintenance with milder agents. In sum, fluocinolone’s molecular architecture translates into a potent yet controllable immunomodulatory tool, provided clinicians respect its pharmacodynamic nuances and adhere to evidence‑based application protocols.
Marc Clarke
October 19, 2025 AT 07:00Totally agree with the deep dive-what’s awesome is that when you follow the fingertip‑unit rule, you get just enough drug to calm the flare without overdoing it. Keeping the skin moisturized right after the cream dries is a game‑changer, and most folks see the itch drop off in a few days. The key is sticking to the two‑week max and giving your skin a breather. That way you avoid those nasty thin‑skin patches and keep the immune system happy.
angelica maria villadiego españa
October 21, 2025 AT 21:30I’ve been using fluocinolone for my eczema, and the relief is real. The cream feels light and doesn’t leave a greasy film, so it’s easy to apply before bed. I make sure my skin is clean and dry, then just a fingertip‑sized amount does the trick. After a week, the redness faded and the itch stopped driving me crazy. I also keep a gentle fragrance‑free moisturizer handy to keep the skin barrier strong.
Ted Whiteman
October 24, 2025 AT 12:00Sure, the cream works, but let’s not pretend it’s a miracle cure. People love to slap it on everything and ignore the warnings about occlusion and long‑term use. You’ll end up with spider veins and skin that’s as thin as tissue paper if you don’t respect the guidelines. Remember, steroids are powerful tools, not a free‑for‑all. Use them wisely, or you’ll pay the price later.
Dustin Richards
October 27, 2025 AT 01:30From a clinical perspective, it’s essential to distinguish fluocinolone from super‑potent steroids like clobetasol. Fluocinolone offers a safer profile for intermittent use on delicate areas such as the face and intertriginous zones. When prescribing, I emphasize the two‑week limit and recommend a tapering strategy to prevent rebound inflammation. Pairing the steroid with an occlusive‑free moisturizer helps restore the lipid barrier and reduces the risk of atrophy. Monitoring for signs of adrenal suppression, especially in pediatric patients, remains a critical safety measure.
Vivian Yeong
October 29, 2025 AT 16:00Short‑term use is fine, but overuse can cause skin thinning.
suresh mishra
November 1, 2025 AT 06:30Fluocinolone’s fluorine atom enhances glucocorticoid receptor binding, which translates into a stronger anti‑inflammatory response while maintaining relatively low systemic absorption when used properly.
Reynolds Boone
November 3, 2025 AT 21:00That binding boost means you get quicker symptom relief, but it also underscores why we must limit the treatment window. The faster you see results, the less temptation there is to keep applying it beyond the recommended period. Keeping a simple log of itch intensity can help you decide when to stop.
Tony Halstead
November 6, 2025 AT 11:30Think of fluocinolone as a well‑tuned instrument in the orchestra of skin health. When played with precision-light application, short intervals-it harmonizes the immune response without drowning out the skin’s natural resilience. Yet, if you overplay, the melody turns discordant, leading to atrophy and barrier breakdown. The art lies in knowing when to let the instrument rest, allowing the skin’s own reparative rhythms to resume. In practice, this translates to a mindful regimen: cleanse, apply a pea‑sized dab, moisturize, and then step back. By respecting the cadence, you keep the skin’s symphony in tune.
leo dwi putra
November 9, 2025 AT 02:00Whoa, you’re turning a cream into a concerto? Sure, that’s poetic, but let’s keep it real-people aren’t going to read a sonnet before slathering on the stuff. The bottom line is simple: use a thin layer, don’t cover it up, and give your skin a break. If you ignore that, you’ll see those dreaded spider veins faster than a pop‑star’s Instagram follower count.
Krista Evans
November 11, 2025 AT 16:30Hey team, let’s keep the vibe positive! If you’ve got a flare, remember the two‑week rule and pair your fluocinolone with a fragrance‑free moisturizer. It’ll help lock in hydration and keep that skin barrier strong. You’ve got this-stay consistent, track your progress, and you’ll be back to feeling comfortable in no time.
Mike Gilmer2
November 14, 2025 AT 07:00Alright, let’s get dramatic for a sec-imagine a world where everyone just waved a magic wand and vanished their rashes. Spoiler: it’s not that easy. Fluocinolone is your backstage pass to relief, but only if you respect the curtain call. Apply, retreat, repeat the cycle-no encores, no over‑the‑top performances.
Alexia Rozendo
November 16, 2025 AT 21:30Oh great, another skincare routine. Because we all have time to log itch scores and count fingertip units. Sure, follow the guidelines, but at the end of the day, it’s just a cream-don’t let the hype scare you off.
Millsaps Mcquiston
November 19, 2025 AT 12:00Let’s cut the drama. This cream works, it’s backed by science, and if you follow the simple steps-apply a thin layer, avoid covering it up, and stop after two weeks-you’ll avoid the nasty side effects. No need to overcomplicate it; just do what the doctors say.