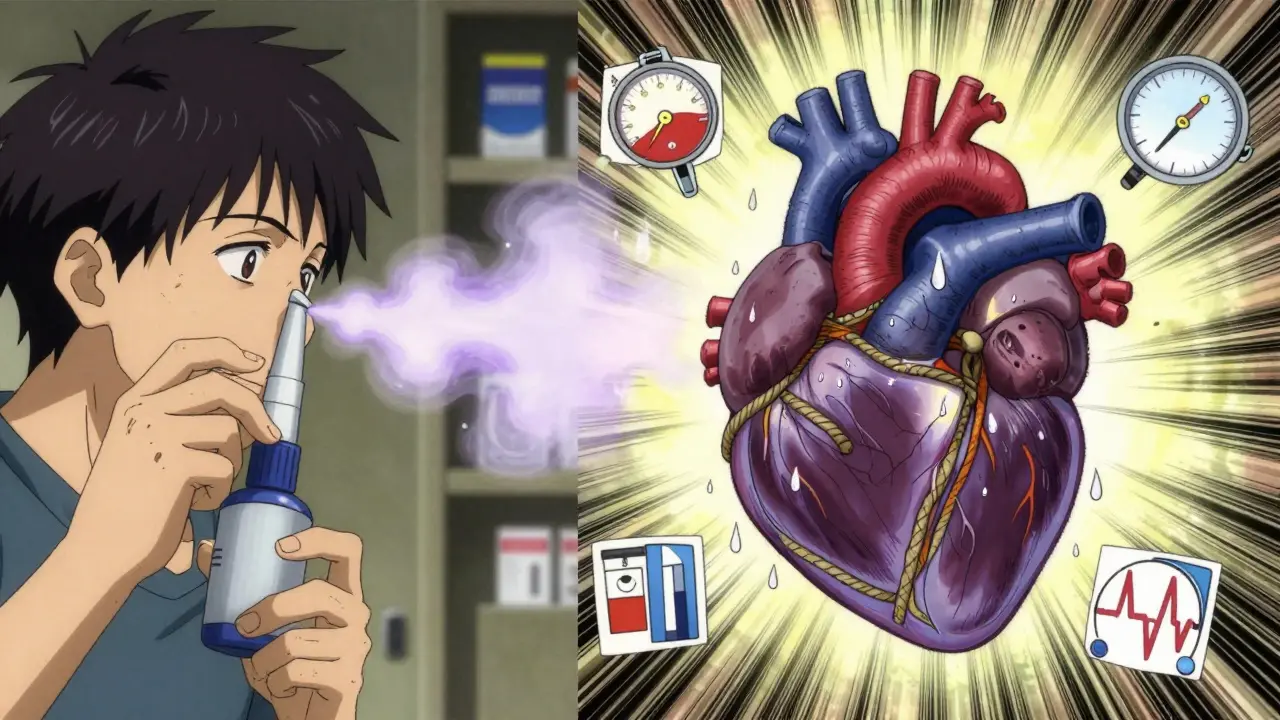
If you have heart disease or high blood pressure, taking a common cold medicine could be riskier than you think. Decongestants like pseudoephedrine and phenylephrine are everywhere-on pharmacy shelves, in multi-symptom cold pills, even in nasal sprays. They promise quick relief from a stuffy nose. But for people with heart conditions, that relief comes with a hidden cost: decongestants can push blood pressure higher, trigger irregular heartbeats, and in rare but serious cases, lead to heart attacks or heart failure.
How Decongestants Work-and Why That’s Dangerous for Your Heart
Decongestants shrink swollen blood vessels in your nose to reduce congestion. That’s why they work. But they don’t just target your nasal passages. These drugs, especially oral ones like pseudoephedrine (Sudafed) and phenylephrine, enter your bloodstream and tighten blood vessels all over your body. That’s called vasoconstriction. For someone with healthy arteries, this might cause a tiny, temporary spike in blood pressure. For someone with heart disease, it’s a different story.
When your blood vessels constrict everywhere, your heart has to work harder to pump blood. Your blood pressure rises. Your heart rate can jump. If you already have narrowed arteries, high blood pressure, or a weakened heart, this extra strain can push your system past its limit. Studies show that even a small increase in systolic pressure-like 5 to 10 mmHg-can significantly raise the risk of cardiac events in vulnerable people.
Who’s at the Highest Risk?
Not everyone with heart trouble needs to avoid decongestants entirely-but some groups should steer clear completely. Medical experts agree on four high-risk categories:
- Uncontrolled high blood pressure (hypertension)
- Heart failure
- History of heart attack or stroke
- Prinzmetal angina (coronary artery spasms)
Even if your blood pressure is usually stable, being sick puts extra stress on your heart. Fighting a cold or flu raises your heart rate and causes inflammation. Add a decongestant on top of that, and you’re stacking risks. The American Heart Association says it plainly: people with uncontrolled hypertension or heart disease should not take oral decongestants.
There’s also the issue of hidden doses. Many cold and flu products combine decongestants with pain relievers, antihistamines, or cough suppressants. You might think you’re just taking something for your cough-but you’re also getting pseudoephedrine. Reading labels isn’t optional. It’s life-saving.
Oral vs. Nasal: Which Is Worse?
Not all decongestants are the same. Oral versions like pseudoephedrine and phenylephrine are absorbed into your bloodstream and affect your whole body. That’s why they carry the strongest warnings. A 2005 meta-analysis found that pseudoephedrine consistently causes a small but measurable rise in systolic blood pressure-enough to matter for people with heart disease.
Nasal sprays like oxymetazoline (Afrin) or naphazoline are supposed to be safer because they’re local. But they’re not risk-free. A 2015 case report described a 40-year-old man who developed a life-threatening hypertensive crisis after overusing a nasal spray containing naphazoline. He had no prior heart issues-but the spray, used too often and too much, triggered heart failure. Even topical decongestants can enter the bloodstream in high doses or with prolonged use.
And here’s the catch: people often use nasal sprays longer than they should. The label says “use for no more than 3 days.” But when congestion lingers, many keep using it. That’s when the risks start piling up.
What the Experts Say
Doctors and medical organizations are united on this: avoid decongestants if you have heart disease or uncontrolled high blood pressure.
The Mayo Clinic says: “Do not take a decongestant if you have severe or uncontrolled high blood pressure.”
Harvard Health acknowledges that the blood pressure rise from pseudoephedrine is small in people with well-controlled hypertension-but warns it becomes dangerous when blood pressure is already too high.
The European Journal of General Medicine puts it bluntly: decongestants don’t treat the cold or allergy-they just mask symptoms. And in people with heart conditions, the risks outweigh the benefits.
Pharmacists play a key role in safety. In Australia and the U.S., pseudoephedrine is kept behind the counter. You have to ask for it. That’s not to make it harder to get-it’s to give the pharmacist a chance to ask, “Do you have high blood pressure? Heart problems?” That question could prevent a hospital visit.
What Can You Use Instead?
You don’t need decongestants to feel better. There are safer, effective alternatives:
- Saline nasal sprays-saltwater rinses clear mucus without affecting blood pressure.
- Humidifiers-adding moisture to the air reduces congestion naturally.
- Guaifenesin (Mucinex)-this expectorant helps thin mucus without constricting blood vessels.
- Steam inhalation-a warm shower or bowl of hot water with a towel over your head can loosen congestion.
- Rest and hydration-your body heals faster when it’s not stressed.
If you need pain relief, acetaminophen (paracetamol) is generally safer than NSAIDs like ibuprofen, which also carry heart risks. Always check with your doctor or pharmacist before taking anything new.

Real Cases, Real Consequences
These aren’t hypothetical risks. There are documented cases of people ending up in emergency rooms because of decongestants.
A 5-year-old girl developed high blood pressure after taking phenylephrine for a cold. Her blood pressure stayed elevated for days-until doctors stopped the medication. No other cause was found.
A 40-year-old man used nasal spray too long and too often. He ended up in cardiac arrest from heart failure triggered by the decongestant. He survived-but it was a close call.
These aren’t rare. They’re preventable.
When in Doubt, Skip It
Decongestants give you a quick fix. But they don’t cure anything. They just hide symptoms while your body fights the infection. If you have heart disease or high blood pressure, your body doesn’t need extra stress. Let it heal without chemical interference.
That means skipping the multi-symptom cold pills that hide decongestants. It means reading every label-even the small print. It means asking your pharmacist: “Is this safe for someone with heart disease?”
There’s no shame in choosing a slower, safer path. In fact, it’s the smartest thing you can do.
Bottom Line
If you have heart disease, high blood pressure, or a history of stroke or heart attack, avoid oral decongestants like pseudoephedrine and phenylephrine. Even nasal sprays can be risky if used too long or too often. Stick to saline rinses, humidifiers, and rest. If symptoms persist, see your doctor. Don’t let a stuffy nose put your heart at risk.



Amy Ehinger
January 15, 2026 AT 09:23I used to think decongestants were harmless until my dad had a near-miss after taking Sudafed for a cold. He didn’t even know he had high blood pressure until then. Now we read every label like it’s a legal contract. Funny how the thing that’s supposed to help you breathe can make your heart feel like it’s trying to escape your chest.
Crystel Ann
January 16, 2026 AT 21:09So many people don’t realize how much stress a cold puts on the body. Rest, hydration, steam-those are the real medicine. Decongestants are like putting a bandaid on a broken engine. It might seem fine for a minute, but you’re just delaying the crash.
Jan Hess
January 18, 2026 AT 16:06Just because you can buy it doesn’t mean you should use it. I always ask my pharmacist before grabbing anything with pseudoephedrine. They’ve saved me more than once. Seriously, talk to the person behind the counter. They know more than the label does.
Sarah Mailloux
January 19, 2026 AT 01:24My grandma used saline spray and a humidifier for everything. She’s 82 and still walks two miles a day. No pills. No drama. Just simple stuff that works without wrecking your insides. Maybe we’ve forgotten how to let our bodies heal.
Nat Young
January 20, 2026 AT 11:59Look I get the fearmongering but this is just Big Pharma pushing saline sprays because they can’t patent them. The real risk is from NSAIDs and acetaminophen, not decongestants. People are dying from liver failure from Tylenol every year but nobody’s banning it. Double standards much?
Niki Van den Bossche
January 21, 2026 AT 08:00Decongestants are the pharmaceutical equivalent of a toxic relationship-temporary relief at the cost of your long-term equilibrium. We’ve been conditioned to believe that symptoms are enemies to be eradicated, not messengers whispering that we’ve ignored our body’s rhythm for too long. The nasal spray is not the villain; it’s the mirror.
Jami Reynolds
January 22, 2026 AT 17:56Let me be perfectly clear: this isn’t about heart disease. This is about the slow, calculated erosion of personal autonomy by the medical-industrial complex. Pseudoephedrine is kept behind the counter not because it’s dangerous-it’s because they want to control your access to natural remedies. The same people who sell you this fear also sell you the ‘safe’ alternatives. Coincidence? I think not.
Did you know the FDA approved phenylephrine despite studies showing it’s no better than placebo? That’s not incompetence. That’s corruption. The pharmaceutical lobby owns the regulatory bodies. Your ‘safe’ saline spray? Probably funded by the same companies that profit from decongestants. Wake up.
They want you dependent. They want you afraid. They want you to believe you need their pills to survive a cold. But the truth? Your body has been healing itself for 3 billion years without a single patent.
And don’t even get me started on ‘pharmacists asking questions.’ That’s not care-that’s surveillance. They’re logging your purchases. Your data is being sold. Your health is being monetized. Read the fine print on the bottle. The real danger isn’t in the medicine-it’s in the system that sells it.
Next time you reach for Sudafed, ask yourself: who benefits? Not you. Not your heart. Someone in a suit with a quarterly earnings report.
Iona Jane
January 23, 2026 AT 15:11They’re lying to us. Every single one of them. The ‘3-day limit’ on nasal sprays? A joke. The real reason they say that is because if you use it longer, your body becomes dependent and you need more. And guess what? That’s how they make money. You think they care if you have heart failure? No. They care if you keep buying. They’re not doctors. They’re merchants. And you’re the product.
I had a friend who used Afrin for 11 months straight. She didn’t even know she was addicted. Then one morning she collapsed. They said it was a hypertensive crisis. But I know. It was the system. The system that sells you poison wrapped in a ‘safe’ label.
Haley Graves
January 23, 2026 AT 23:11Reading this made me realize how much I’ve been ignoring my own heart health. I used to grab whatever cold medicine was on sale. Now I ask my doctor before I touch anything. It’s not about being paranoid-it’s about being responsible. You owe it to yourself to know what you’re putting in your body. Small changes save lives.
Nilesh Khedekar
January 24, 2026 AT 08:51Interesting how Western medicine always seeks a chemical fix, while Ayurveda and Traditional Chinese Medicine have used steam, salt, and rest for millennia. Perhaps the answer isn’t in the bottle-but in the wisdom we’ve discarded. The body knows how to heal. We just keep giving it more work to do.
Nicholas Urmaza
January 26, 2026 AT 08:07It is important to recognize that the cardiovascular risks associated with decongestants are well documented in peer-reviewed literature. The American Heart Association guidelines are not suggestions-they are evidence-based recommendations. Ignoring them is not bravery. It is negligence. Your health is not a gamble.
Gloria Montero Puertas
January 27, 2026 AT 10:57Let’s be honest-most people who take decongestants don’t even understand what vasoconstriction means. They see ‘relieves congestion’ and assume it’s harmless. The average consumer is a walking liability. This isn’t about health. It’s about education. And we’ve failed. Spectacularly.
Pharmacists aren’t the problem. The public’s ignorance is. You don’t need a degree to read a label. You just need to care. And most people don’t. They want fast. They want easy. They want magic. There is no magic. There is only biology.
Dan Mack
January 28, 2026 AT 03:02They’re all lying. The whole system is rigged. Decongestants are fine. The real danger is the blood pressure meds they push you onto after you have a reaction. That’s where the real money is. You think they want you healthy? No. They want you on lifelong pills. That’s the real scam. This whole article is just a gateway to sell you more drugs.
RUTH DE OLIVEIRA ALVES
January 30, 2026 AT 01:34It is a matter of considerable public health significance that the prevalence of self-medication with over-the-counter decongestants remains high among individuals with preexisting cardiovascular conditions. The disconnect between clinical recommendations and consumer behavior reflects a broader failure in health literacy. The responsibility for informed decision-making rests not solely with the physician or pharmacist, but with the individual who ingests the substance. One must recognize that symptom suppression is not therapeutic intervention. The physiological consequences of systemic vasoconstriction in the context of compromised cardiac function are neither theoretical nor anecdotal-they are quantifiable, documented, and entirely preventable.
It is therefore imperative that public health messaging evolve from mere cautionary notes to structured educational frameworks that empower patients to interpret pharmaceutical labeling with precision. The omission of critical warnings on multi-symptom formulations is not merely negligent-it is ethically indefensible. The burden of comprehension should not fall upon the sick, the elderly, or the overwhelmed. It must be borne by the institutions that profit from their vulnerability.
Saline irrigation, humidification, and hydration are not ‘alternatives.’ They are the foundational principles of physiological support. To elevate chemical intervention above these is to misunderstand the very nature of healing. The body is not a machine to be fixed. It is a system to be supported.
Let us not confuse convenience with safety. Let us not mistake accessibility for appropriateness. And let us never forget: the most powerful medicine is often the one we choose not to take.
Jan Hess
January 31, 2026 AT 04:46My mom’s cardiologist told her to avoid decongestants completely. She switched to saline spray and now she actually sleeps through the night. No more racing heart. No more anxiety. Just breathing. Sometimes the best thing you can do is nothing at all.
Nicholas Urmaza
January 31, 2026 AT 12:51That’s exactly right. The body heals when given space. Not when flooded with stimulants disguised as relief. The real win is listening.