When you pick up a generic pill at the pharmacy, you expect it to work just like the brand-name version-same active ingredient, same effect, same safety. But what if that pill was contaminated with a carcinogen? What if the dose was so low it did nothing at all? These aren’t hypotheticals. They’re happening right now, and the people most affected are the ones who rely on generics because they can’t afford the brand names.
What’s Really in Your Generic Medication?
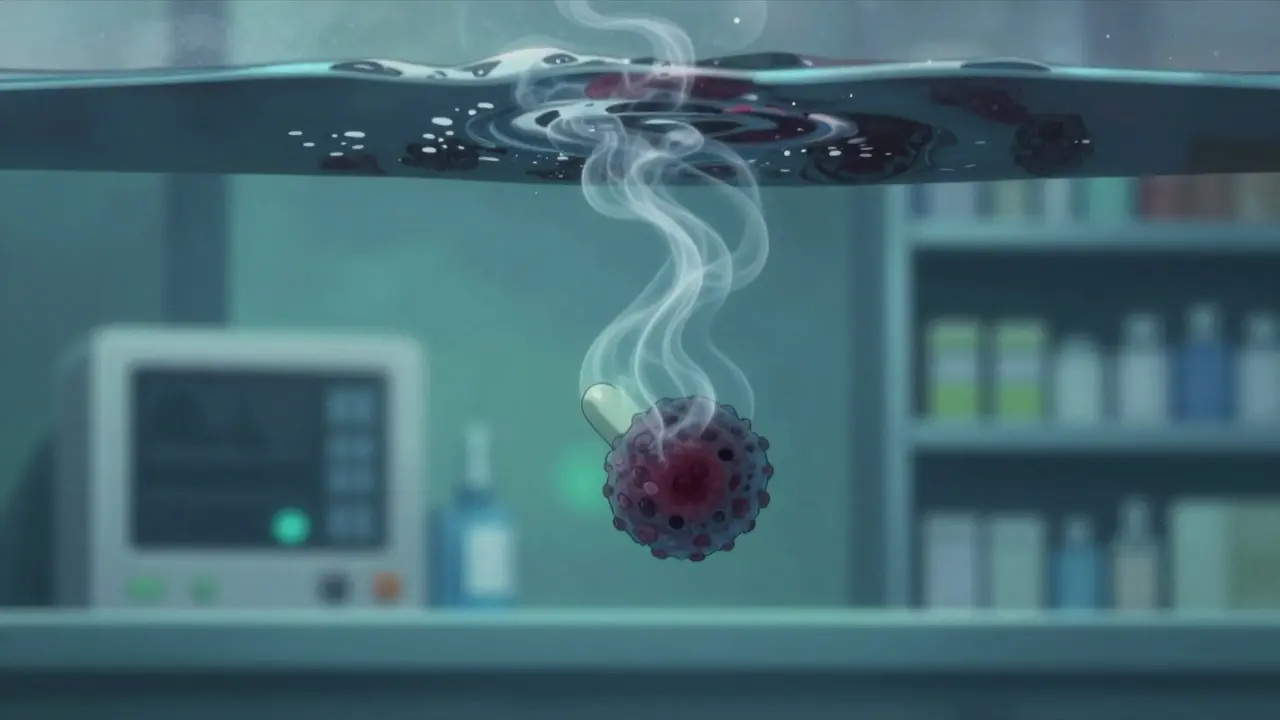
Generic drugs make up 92% of all prescriptions filled in the U.S. They save the healthcare system over $1.7 trillion every decade. But that cost savings comes with a hidden price. Between 2018 and September 2025, the FDA recorded more than 8,000 drug recalls-37% more than the year before. And contamination is the leading cause. One of the worst cases involved valsartan, a blood pressure drug. In 2018, tests found NDMA-a known human carcinogen-in batches made by Zhejiang Huahai Pharmaceutical in China. The levels were up to 200 times higher than the FDA’s safe limit of 96 nanograms per day. Patients who took it for years saw their risk of colorectal cancer jump from 4 cases per 100,000 people to 27 per 100,000. Over 1,300 lawsuits are still active as of late 2025, with some victims diagnosed with cancer just five years after exposure. Then there’s Mucinex. In June 2025, a lawsuit filed in Chicago revealed benzene-a chemical linked to leukemia-was found in some generic versions at 4.7 parts per million. The FDA’s limit is 2 ppm. Independent testing confirmed it. Two women who took the medication daily for 18 months developed bone marrow damage consistent with benzene poisoning. Their stories aren’t rare. They’re symptoms of a broken system.Chemotherapy Drugs That Don’t Work
Cancer patients are among the most vulnerable. A STAT News investigation in June 2025 found that 17 chemotherapy drugs from Indian manufacturers failed basic quality tests. Twelve of them contained less than 80% of the labeled active ingredient. The FDA requires 85-115%. That means a patient getting a 100mg dose might only get 70mg. In one case at Memorial Sloan Kettering, 7 out of 11 patients receiving contaminated cisplatin didn’t go into remission. The same patients, when switched to verified brand-name versions, responded normally. The manufacturer behind many of these failures? Intas Pharmaceuticals in Ahmedabad. An FDA inspection in December 2022 found workers shredding quality control documents and pouring acid on them. No one was held accountable. By spring 2023, 92% of U.S. cancer centers reported shortages of critical chemotherapy drugs. Patients were forced to delay treatment. Some died waiting.Leaky Fentanyl Patches and the Risk of Overdose
Opioid contamination is terrifying because it’s invisible until it’s too late. Between 2002 and September 2025, over 52 million fentanyl patches were recalled due to seal failures. One recall by Sandoz in 2023 affected 1.2 million Duragesic patches. Testing showed 0.8% of them leaked more than 15% of their intended dose. That’s enough to kill someone who’s never used opioids before. Emergency rooms reported a spike in overdoses tied to these patches. Patients thought they were getting steady pain relief. Instead, they were getting sudden, lethal doses. Doctors didn’t know which batches were bad. The FDA didn’t tell them. That’s because, until recently, the agency routinely redacted the names of drugs linked to foreign facility violations. Patients and providers were flying blind.
Why Is This Happening?
The problem isn’t just bad actors-it’s a system designed for speed over safety. The 1984 Hatch-Waxman Act made it easier to approve generics by letting manufacturers prove bioequivalence instead of running full clinical trials. That was smart at the time. But today, with over 10,000 approved generic products and 40% of U.S. generics made in India, the system is overwhelmed. India produces 20% of the world’s generic drugs. Yet the FDA inspects only 13% of Indian plants each year. There are over 28,000 foreign manufacturing facilities that need inspection. The FDA’s 2025 budget for foreign inspections? $78 million. That’s enough for 1,200 inspections. Not even close. Worse, 83% of the top 100 generic drugs sold in the U.S. contain active ingredients made in China or India. No U.S. sourcing. No traceability. No accountability. When a batch fails, you can’t always tell where it came from. And even when you can, the FDA often doesn’t name the company in public reports.What’s Being Done-and Why It’s Not Enough
The FDA launched its Pharmaceutical Quality for the 21st Century initiative in 2011 to push for better manufacturing controls. It encouraged real-time monitoring, automated testing, and continuous production. But as of 2025, only 37% of foreign facilities use these tools. In India, it’s just 3%. New rules under GDUFA III, effective June 2025, now require real-time stability testing for high-risk drugs like chemotherapy and blood pressure medications. That’s progress. But enforcement is still weak. The FDA can issue warning letters, but rarely shuts down plants permanently. Zhejiang Huahai, the company behind the valsartan NDMA scandal, was cited again in April 2025-for destroying documents. They’re still making drugs. The Drug Supply Chain Security Act requires full electronic tracking of every drug package by 2027. But right now, only 62% of pharmacies can verify if a drug is legitimate. Pharmacists are spending 22% more time checking recall lists. One pharmacist in Ohio told Pharmacy Times: “I’ve seen three different batches of generic levothyroxine fail potency tests in six months. Patients’ thyroid levels went wild until we switched back to brand.”
How to Protect Yourself
You can’t control what’s in the bottle-but you can make smarter choices.- Ask your pharmacist: “Is this generic from a U.S.-based manufacturer?” Some pharmacies stock multiple versions. They can tell you which ones have better track records.
- Check the FDA’s recall list every month. Go to fda.gov/drugs/drug-safety-and-availability/drug-recalls. Bookmark it. It’s free and updated daily.
- Monitor your body: If your blood pressure suddenly spikes after switching to a new generic, or your pain isn’t controlled, or you feel unusually tired-talk to your doctor. It might not be your condition. It might be your drug.
- Consider brand when it matters: For drugs where tiny differences matter-thyroid meds, seizure meds, blood thinners, chemotherapy-brand-name versions often have tighter quality control. If you can afford it, or if your insurance covers it, it might be worth it.
The Bigger Picture
This isn’t just about pills. It’s about trust. When you take a drug, you’re trusting the system to keep you safe. But the system is stretched thin, underfunded, and too reliant on overseas factories with little oversight. The FDA’s new “Name Transparency Initiative,” announced in September 2025, promises to stop hiding drug names in inspection reports. That’s a step forward. But without real penalties-fines that hurt, plant closures that stick, criminal charges for falsifying records-the problem won’t end. The Valsartan lawsuits may set a legal precedent. If courts find manufacturers knowingly hid contamination risks, it could change everything. But until then, patients are the ones paying the cost-in health, in money, in lives.What’s Next?
The FDA’s 2026-2030 plan aims to cut contamination recalls by 50% using AI and blockchain tracking. That sounds promising. But experts like Dr. Dinesh Thakur, a former pharma insider turned whistleblower, aren’t convinced. “Without meaningful penalties,” he says, “the problem will continue.” And he’s right. Technology won’t fix a system that doesn’t care enough to enforce the rules. Until the cost of cutting corners is higher than the cost of doing it right, contamination will keep happening. You deserve safe medicine. No matter your income. No matter your insurance. That’s not a luxury. It’s a right.Are generic drugs always safe?
Most generic drugs are safe and effective. But contamination incidents have increased sharply since 2018, with over 8,000 recalls linked to impurities, incorrect dosing, or manufacturing defects. While the majority of generics are fine, high-risk drugs like chemotherapy, blood pressure meds, and opioids have seen repeated failures. Always check the FDA recall list and ask your pharmacist about the manufacturer.
What drugs have been most affected by contamination?
Blood pressure medications (especially ARBs like valsartan) account for 28% of contamination-related recalls since 2018. Oncology drugs like cisplatin and carboplatin make up 19%, and respiratory drugs like Mucinex (with benzene) account for 14%. Fentanyl patches have had over 52 million recalled due to seal failures. These are the categories where contamination has had the most serious health consequences.
Can I trust generics made in India or China?
Many generics made in India and China are safe and meet standards. But inspection rates are extremely low-only 13% of Indian facilities are checked annually, despite supplying 40% of U.S. generics. Some manufacturers have repeated violations. Zee Laboratories has been flagged 46 times since 2018. If you’re on a critical medication, ask your pharmacist if the generic is made by a U.S.-based or better-rated manufacturer.
How do I know if my generic drug is contaminated?
You usually can’t tell by appearance or how you feel. Contaminants like NDMA or benzene don’t cause immediate symptoms. The best way is to check the FDA’s recall database monthly and monitor for unexpected changes in your condition-like unexplained fatigue, abnormal blood tests, or worsening symptoms after a new prescription. If something feels off, talk to your doctor and ask for a different batch or brand.
Should I avoid generics altogether?
No. Generics are essential for affordable care. Over 90% of prescriptions are filled with them. But for drugs where precision matters-thyroid meds, epilepsy drugs, chemotherapy, or opioids-it’s worth considering brand-name versions if you can afford them or if your insurance covers them. The difference in quality control can be life-changing.
What’s being done to fix this?
The FDA introduced new rules in 2025 requiring real-time testing for high-risk drugs and plans to stop hiding drug names in inspection reports. They’re also testing AI and blockchain for supply chain tracking by 2030. But enforcement remains weak. Only 3% of Indian plants use modern manufacturing tech. Until penalties are severe and inspections are frequent, the risk will remain.


Jillian Angus
December 24, 2025 AT 17:57Just saw my last prescription for levothyroxine was from a batch recalled last week. I had no idea. My doctor never mentioned it. I just thought I was getting worse.
Gray Dedoiko
December 24, 2025 AT 18:01This is terrifying. I take generic blood pressure meds because I'm on a fixed income. I never thought about where they came from. I just trusted the label. Now I'm scared to take them.
Aurora Daisy
December 26, 2025 AT 02:19Oh great. So now we're outsourcing poison to India and China because we're too lazy to make medicine here. Classic American capitalism. Let someone else die so we can save $3.47.
CHETAN MANDLECHA
December 27, 2025 AT 17:44As someone from India, I’m deeply ashamed. Many small manufacturers cut corners because the global market demands lower prices. But this isn’t just about profit-it’s about lives. We need systemic reform, not finger-pointing.
Bhargav Patel
December 27, 2025 AT 22:42The fundamental flaw lies not in the manufacturing per se, but in the epistemological surrender of regulatory authority to economic efficiency. The Hatch-Waxman Act was predicated on a model of equivalence that assumed homogeneity in production ethics-a naive assumption in a globalized supply chain where oversight is commodified. The FDA’s budgetary constraints are not merely fiscal; they are moral failures encoded in policy.
When we outsource not just labor but accountability, we create systems where compliance becomes performative. The shredding of documents, the acid baths, the falsified logs-they are not anomalies. They are logical outcomes of a system that measures success by cost per unit, not lives preserved.
AI and blockchain may offer traceability, but without punitive consequences that cripple corporate incentives, they are digital bandages on a hemorrhaging wound. The real solution is not technological-it is political. We must demand that the FDA be funded as if human life is non-negotiable.
And yet, we continue to elect leaders who treat pharmaceuticals like widgets. We are not victims of contamination. We are victims of indifference.
Charles Barry
December 28, 2025 AT 12:41Let me guess-the FDA is in bed with Big Pharma. They’re hiding the names because they know the same companies that made the contaminated drugs are the ones funding their next budget. This isn’t negligence. It’s collusion. The ‘Name Transparency Initiative’? A PR stunt. They’ll name a few minor players and let the big ones walk. I’ve seen this movie before. It always ends with someone’s kid in the ICU.
Rosemary O'Shea
December 30, 2025 AT 10:43Oh, so now we’re supposed to trust the FDA? After they let 1.2 million fentanyl patches leak into the market? After they ignored whistleblower reports for years? This isn’t a public health crisis-it’s a farce. And you, dear author, are just another person with a keyboard pretending to care while the real culprits sip champagne in Zurich.
EMMANUEL EMEKAOGBOR
December 31, 2025 AT 19:23It’s heartbreaking to see how many lives are treated as collateral in the name of affordability. I come from a country where medicine is a luxury, and I’ve seen people ration pills. But this? This is different. This isn’t scarcity-it’s betrayal. The system promised safety. It delivered silence.
Joe Jeter
January 1, 2026 AT 20:20Everyone’s panicking about generics, but have you checked how many brand-name drugs get recalled? Same issues. Same factories. Same regulators. The difference? Brand-name companies charge $500 for a pill so you feel better about paying for it. The real scam isn’t contamination-it’s the illusion of safety behind the fancy packaging.
Sidra Khan
January 2, 2026 AT 09:31So… what’s the point? We can’t afford brand names, we can’t trust generics, and the FDA won’t tell us what’s safe. I’m just gonna stop taking meds and hope I die of something less boring. 💀
Gray Dedoiko
January 3, 2026 AT 17:09My mom switched back to brand-name lisinopril after her BP went haywire. She’s fine now. I know it’s expensive, but if your life depends on it… sometimes you have to bite the bullet. I wish more people knew this wasn’t just about money-it’s about survival.