When a patient gets sick after taking a new medication, how do you know if the drug actually caused the problem? It’s not always obvious. Maybe it was the flu. Maybe it was an old condition flaring up. Or maybe it really was the drug. That’s where the Naranjo Scale comes in. It’s not a fancy machine or a high-tech app. It’s a simple 10-question checklist that helps doctors, pharmacists, and nurses decide if a side effect is truly caused by a medicine - or if something else is to blame.
Why the Naranjo Scale Matters
In the 1960s, thousands of babies were born with severe birth defects after their mothers took thalidomide for morning sickness. That disaster changed everything. It showed the world that drugs can have hidden, dangerous side effects - and that we need better ways to spot them. Since then, drug safety has become a global priority. Every time a patient reports a strange reaction, regulators and hospitals need to know: Is this a real drug reaction? Or just bad luck? That’s where the Naranjo Scale steps in. Developed in 1981 by Dr. Carlos Naranjo and his team, it was the first standardized tool to turn guesswork into a clear, repeatable process. Today, it’s still used in over 75% of hospital pharmacovigilance programs worldwide. It doesn’t require expensive equipment. You don’t need a PhD. All you need is the patient’s chart, a pen, and a basic understanding of how drugs work.How the Naranjo Scale Works
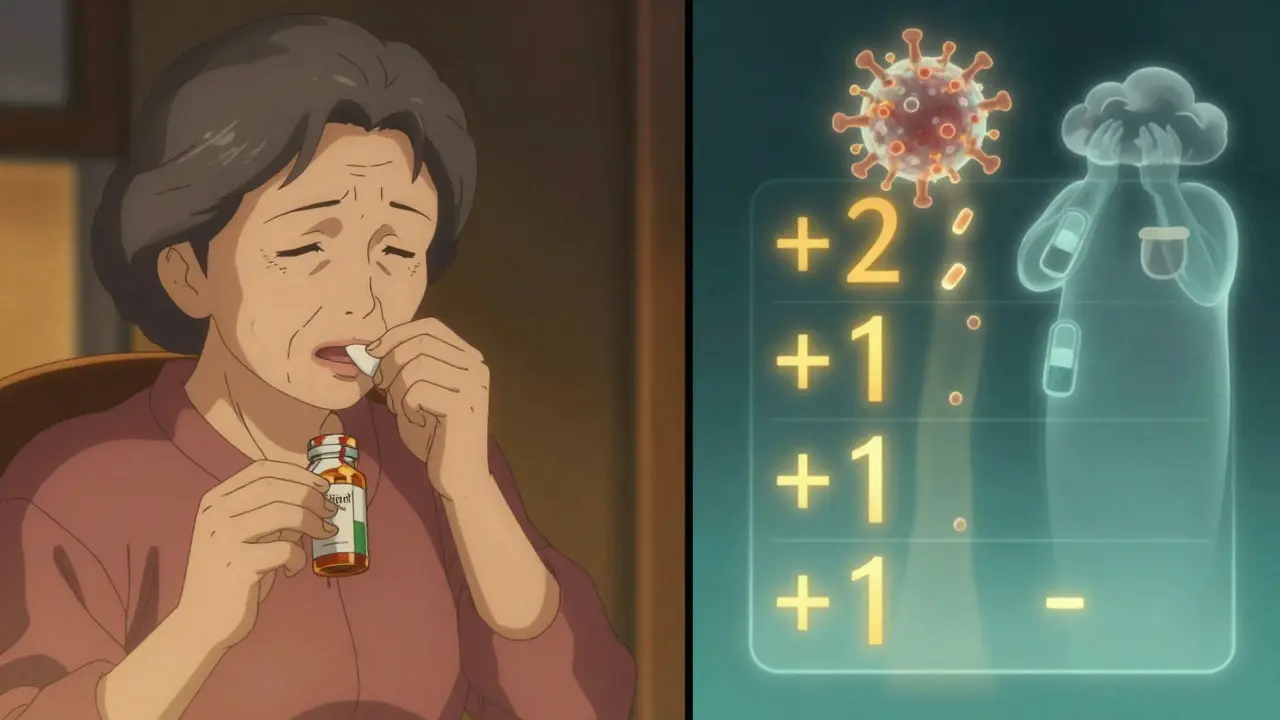
The scale has 10 questions. Each one asks something specific about the patient’s history and the timing of their reaction. For each answer, you give a score: +2, +1, 0, or even -1. The total score tells you how likely it is that the drug caused the problem. Here’s what the questions look like - and what they’re really asking:- Question 1: Has this reaction been reported before with this drug? (+1 if yes)
- Question 2: Did the reaction happen after the drug was started? (+2 if clearly timed, -1 if it happened before)
- Question 3: Did symptoms get better after stopping the drug? (+1 if yes)
- Question 4: Did the reaction return when the drug was given again? (+2 if yes, -1 if it got worse)
- Question 5: Could something else have caused it? (-1 if yes, +2 if no other explanation fits)
- Question 6: Was a placebo used to test if the reaction was real? (-1 if placebo caused it, +1 if it didn’t)
- Question 7: Was the drug level in the blood too high? (+1 if toxic levels were found)
- Question 8: Did the reaction get worse when the dose was increased? (+1 if yes)
- Question 9: Has the patient had this reaction to the same drug before? (+1 if yes)
- Question 10: Is there lab or clinical proof the reaction matches the drug’s known effects? (+1 if confirmed)
That’s it. Ten questions. Simple. But don’t be fooled - answering them right takes experience. For example, Question 5 is the trickiest. If a patient has diabetes and develops swelling after starting a new blood pressure pill, is the swelling from the drug - or from their diabetes getting worse? That’s where clinical judgment comes in.
What the Score Means
After you add up the points, the total tells you the likelihood the drug caused the reaction:- 9 or higher: Definite - The drug almost certainly caused it. The timing fits, symptoms improved after stopping, and no other explanation makes sense.
- 5 to 8: Probable - Likely the drug, but there’s some doubt. Maybe rechallenge wasn’t possible, or there’s a weak alternative cause.
- 1 to 4: Possible - The drug could be involved, but other factors are just as likely. This is common in older patients on multiple drugs.
- 0 or lower: Doubtful - The reaction probably wasn’t caused by the drug. Maybe it was an infection, stress, or another medication.
For example, a 72-year-old woman starts taking lisinopril for high blood pressure. Three days later, she develops a dry cough. Her score: +2 for timing, +1 for improvement after stopping, +1 for known side effect, +1 for previous similar reaction, and -1 because she had a cold last week. Total: 4. That’s “possible.” Not definite - but enough to flag it for monitoring.
How It Compares to Other Tools
There are other ways to assess drug reactions. The WHO-UMC system, used by global health agencies, is simpler. It just says: certain, probable, possible, unlikely. No numbers. But that also means less precision. Two doctors might look at the same case and disagree on whether it’s “probable” or “possible.” The Naranjo Scale is more detailed. Studies show it has better agreement between raters - about 50% more consistent than WHO-UMC. That’s why it’s still the go-to tool in research papers and hospital reporting systems. But it’s not perfect. Here’s where it falls short:- One drug at a time: Most elderly patients take 5-10 medications. The Naranjo Scale can’t handle that. If someone takes aspirin, metformin, atorvastatin, and warfarin - and then gets bleeding - which one caused it? The scale doesn’t help.
- Placebo challenge is unethical: Question 6 asks if a placebo was used to test the reaction. But giving a fake pill to someone who had a dangerous reaction? That’s not done anymore. Most clinicians skip this or mark “don’t know.”
- No room for nuance: It’s all yes/no. What if the reaction was mild? What if the drug was taken irregularly? The scale doesn’t adjust for that.
That’s why newer tools like the Liverpool ADR Scale and PADRAT (for kids) were developed. But none have replaced the Naranjo Scale. Why? Because it’s transparent. You can see every step. You can explain it to a patient. And it’s been tested in over 10,000 real cases.
Real-World Use and Challenges
In hospitals, pharmacists use the Naranjo Scale every day. At Massachusetts General Hospital, they run a daily ADR review. Every suspected reaction gets scored. That data goes into a national database. Without this system, we wouldn’t know that certain antibiotics cause tendon rupture, or that statins can trigger memory loss. But there are problems. One study found that 35% of nurses and doctors disagree on how to score Question 5 - “Are there other possible causes?” That’s a lot of room for error. And rechallenge (Question 4) is often impossible. If a patient had a life-threatening rash, no doctor will give them the drug again. So they mark “don’t know.” That pushes the score down from “definite” to “probable.” That’s why digital tools are catching on. A 2023 study showed that a free Python-based calculator cut assessment time from 11 minutes to 4 minutes. Error rates dropped from 28% to 9%. Some EHR systems like Epic now auto-fill 4 of the 10 questions using patient data - like when the drug was started, or if symptoms improved after stopping.
Is It Still Relevant in 2026?
Yes - but with limits. The Naranjo Scale was built for aspirin, penicillin, and blood pressure pills. It wasn’t designed for biologics, immunotherapies, or gene therapies. These drugs can cause reactions months after stopping. Or they trigger immune responses that look nothing like classic side effects. Experts agree: the Naranjo Scale isn’t enough for modern medicine. But it’s still the best starting point. The FDA and EMA still require it for serious ADR reports. And for 80% of cases - the common ones involving older drugs - it works perfectly. What’s next? A 2024 draft from the International Council for Harmonisation suggests replacing Question 6 (placebo) with a question about therapeutic drug monitoring. That’s a smart update. And AI systems are being trained to predict reactions using huge databases of patient records. But even those systems still use the Naranjo Scale as their training ground.How to Learn It
You don’t need a pharmacology degree to use it. Most nurses and pharmacists learn it in 2-4 hours. The key is practice. Fiveable, a free educational platform, has 12 real-case examples used by over 15,000 students. Start with simple cases: a patient on one new drug, one clear symptom. Score it. Then check the answer. Do it five times. You’ll get it. Many hospitals have printable worksheets. The Nebraska ASAP tool is downloaded over 3,000 times a year. You can find it online. Or use the open-source calculator on GitHub - it’s free, updated in 2023, and runs on any computer.Final Thought
The Naranjo Scale isn’t flashy. It doesn’t use AI. It doesn’t predict the future. But it does something more important: it makes us slow down. It forces us to ask the right questions. It turns a hunch into evidence. In a world full of complex drugs and noisy data, that’s not just helpful - it’s essential.Next time you hear about a side effect, don’t just assume it’s the drug. Ask: What’s the timeline? Did it get better after stopping? Could anything else have caused it? That’s the Naranjo Scale in action - and it’s still the gold standard for a reason.



Jarrod Flesch
January 21, 2026 AT 03:44Ashok Sakra
January 22, 2026 AT 18:44Rod Wheatley
January 23, 2026 AT 04:15michelle Brownsea
January 23, 2026 AT 06:58Glenda Marínez Granados
January 23, 2026 AT 15:05Andrew Rinaldi
January 23, 2026 AT 19:19Yuri Hyuga
January 23, 2026 AT 23:10MAHENDRA MEGHWAL
January 24, 2026 AT 19:59Gerard Jordan
January 25, 2026 AT 03:05Kevin Narvaes
January 25, 2026 AT 19:13Philip Williams
January 27, 2026 AT 07:26