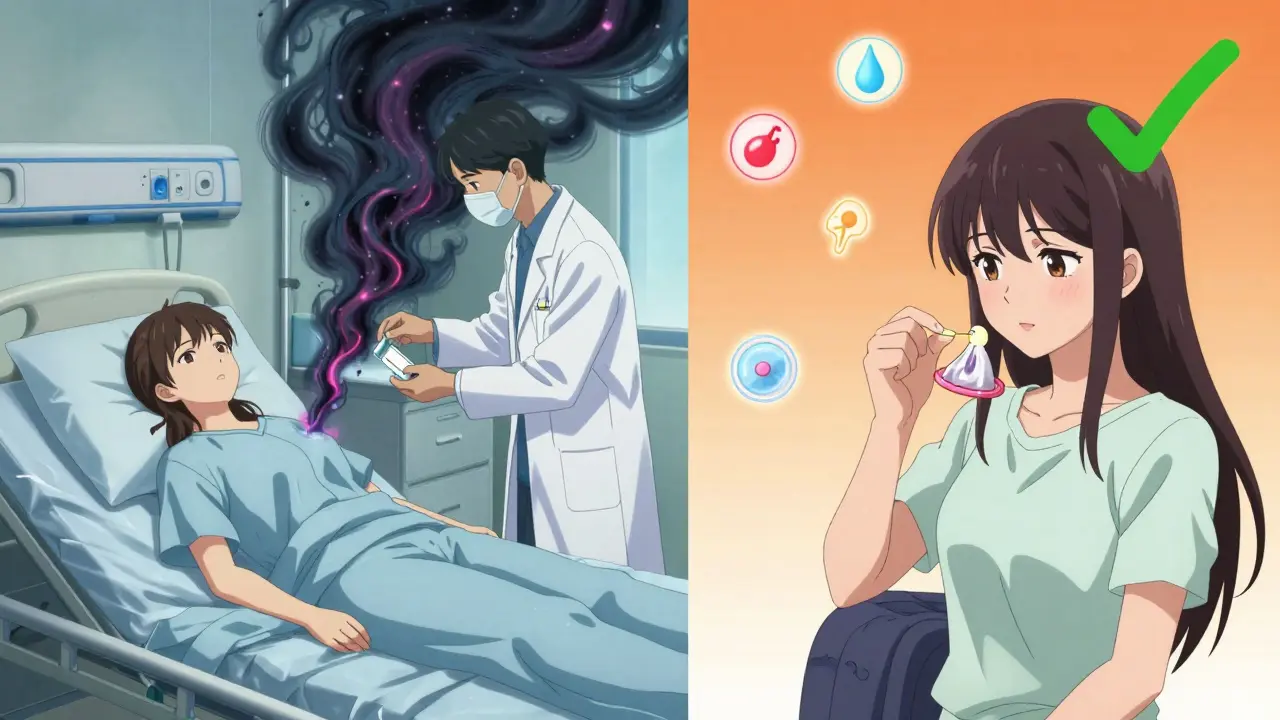
For decades, women have been told: antibiotics can mess with your birth control. If you’ve ever been handed a pamphlet at the pharmacy or heard a friend say, "Just use condoms while you’re on antibiotics," you’re not alone. But here’s the truth: for almost all antibiotics, that advice is outdated. The real risk is tiny - and it only applies to one specific group of drugs.
Most Antibiotics Don’t Touch Birth Control
Let’s clear this up right away: if you’re taking amoxicillin, azithromycin, doxycycline, metronidazole, or ciprofloxacin - the antibiotics most commonly prescribed for sinus infections, UTIs, or strep throat - your birth control pills are still working. There’s no meaningful drop in hormone levels. No increased chance of pregnancy.
Back in the 1970s, a few scattered reports linked birth control failure with antibiotic use. Those stories stuck. But modern science has dug deeper. A 2011 review in the journal Contraception looked at 14 studies and found zero evidence that penicillin-type antibiotics like amoxicillin interfere with how your body absorbs estrogen. Another study from 2020 analyzed 35 clinical trials and confirmed that non-rifamycin antibiotics don’t lower hormone levels below the threshold needed to prevent ovulation.
Think about it: if amoxicillin really reduced birth control effectiveness, we’d see a spike in unplanned pregnancies every flu season. We don’t. The CDC, ACOG, and WHO all agree - for these common antibiotics, no backup method is needed.
The One Antibiotic That Actually Matters
There’s one exception. And it’s not what most people think.
Rifampin (brand name Rifadin) - and its close relative rifabutin - are the only antibiotics with solid, proven evidence of reducing birth control effectiveness. These drugs are used to treat tuberculosis and some other serious infections. They work by turning on liver enzymes that break down hormones faster. Studies show rifampin can slash ethinyl estradiol (the estrogen in most pills) by up to 50%. Progestin levels drop too. That’s enough to let ovulation happen.
The CDC classifies rifampin and rifabutin as Category 3 interactions - meaning the risks outweigh the benefits when used with hormonal birth control. If you’re prescribed one of these, you need backup contraception for 28 days after finishing the course. That’s not a suggestion. It’s a medical requirement.
And here’s a twist: many people confuse rifampin with rifaximin (Xifaxan), which is used for traveler’s diarrhea. Rifaximin does NOT affect birth control. It stays in the gut and doesn’t trigger liver enzymes. Don’t assume all "rif-" drugs are the same.
Other Drugs That Actually Interfere (And What You Should Know)
Antibiotics aren’t the only offenders. Some other medications you might be taking can also lower hormone levels:
- Griseofulvin - an antifungal for nail or skin infections - also speeds up hormone breakdown. Use backup for one month after treatment.
- St. John’s Wort - a popular herbal supplement for mood - can reduce estrogen levels by up to 57%. It’s not an antibiotic, but it’s often taken without knowing the risk.
- Lamotrigine (at doses over 300 mg/day) and topiramate (over 200 mg/day) - used for epilepsy or migraines - interfere with birth control too.
- Some HIV meds like efavirenz and nevirapine also reduce hormone concentrations.
If you’re on any of these, talk to your doctor. Don’t rely on guesswork. Your birth control might still work - but it’s not worth the gamble.
Why Does the Myth Still Exist?
So why are so many people still scared? Partly because of old habits. Pharmacists, doctors, and even online forums still repeat the warning - even when it’s not needed. A 2022 study found that 35% of pharmacists still advise backup contraception for all antibiotics. That’s not based on current evidence. It’s just what they were taught years ago.
Another reason? Fear. When something important like birth control fails, people look for a reason. Antibiotics are easy to blame. But studies show most cases of birth control failure during antibiotic use were due to missed pills, vomiting, or - in rare cases - rifampin. Not amoxicillin.
Dr. Jen Gunter, an OB/GYN and author of The Menopause Manifesto, puts it bluntly: "There’s zero evidence that common antibiotics like amoxicillin affect birth control." And yet, social media is full of stories like, "I got pregnant while on antibiotics." Those stories are real - but they’re almost always tied to something else.
What Should You Do?
Here’s your simple guide:
- If you’re on amoxicillin, azithromycin, doxycycline, ciprofloxacin, metronidazole, or most other common antibiotics - no change needed. Keep taking your pill. No backup required.
- If you’re on rifampin or rifabutin - use condoms or another barrier method for 28 days after your last dose. Talk to your doctor about switching to a non-hormonal option during treatment.
- If you’re on griseofulvin, St. John’s Wort, lamotrigine, topiramate, or certain HIV meds - use backup contraception. These are real risks.
- If you’re unsure - ask your pharmacist or doctor to check your specific combo. Bring a list of everything you’re taking.
And remember: if you miss a pill, vomit within two hours of taking it, or have diarrhea for more than 48 hours - those are the real red flags. Not the antibiotic.

What About the Patch or Ring?
Same rules apply. Rifampin and rifabutin reduce hormone levels in the patch and vaginal ring too. The CDC says backup contraception is needed for 28 days after these drugs - no matter which hormonal method you use.
But again: if you’re on the patch or ring and taking amoxicillin for a sinus infection? You’re fine. No extra steps.
What’s Next?
Medical guidelines keep updating. In January 2023, the FDA updated labels on all hormonal contraceptives to clearly state: "Rifampin, rifabutin, and griseofulvin may reduce effectiveness. Other antibiotics do not." That’s a big deal. It means manufacturers are now legally required to reflect the science.
Still, there’s work to do. A 2023 survey of 500 OB/GYNs found 98% agreed only rifamycins require backup. But 35% of pharmacists still overwarn. That gap is where confusion lives.
For patients, the takeaway is simple: don’t panic. Don’t assume. Ask. And know this - your birth control isn’t broken just because you took an antibiotic for a sore throat.
Do all antibiotics reduce the effectiveness of birth control pills?
No. Only two types of antibiotics - rifampin and rifabutin - have been proven to reduce hormone levels enough to risk contraceptive failure. These are used to treat tuberculosis and some serious infections. Common antibiotics like amoxicillin, azithromycin, doxycycline, and metronidazole do not affect birth control pills.
Is it safe to take amoxicillin while on birth control?
Yes. Amoxicillin does not interfere with hormonal birth control. Multiple studies, including a 2011 review in Contraception and a 2020 CDC analysis of 35 clinical trials, confirm that amoxicillin and similar penicillin-class antibiotics do not lower estrogen or progestin levels to a point that would cause ovulation. No backup contraception is needed.
What should I do if I’m prescribed rifampin?
Use a backup method of contraception - like condoms or a diaphragm - for 28 days after your last dose of rifampin. This applies to all hormonal methods, including pills, patches, and vaginal rings. Talk to your doctor about alternative birth control options during this time, as the interaction is well-documented and significant.
Can St. John’s Wort affect birth control?
Yes. St. John’s Wort, a herbal supplement often used for mild depression, can reduce estrogen levels by up to 57%, according to a 2017 study in Clinical Pharmacology & Therapeutics. It’s not an antibiotic, but it’s a known drug interaction. If you’re taking it, use backup contraception or switch to a non-hormonal birth control method.
I got pregnant while on antibiotics. Was it the antibiotics?
It’s very unlikely unless you were taking rifampin or rifabutin. Most cases of pregnancy during antibiotic use are due to missed pills, vomiting, diarrhea, or taking other interacting drugs like St. John’s Wort or certain seizure medications. Antibiotics like amoxicillin or azithromycin are not the cause. If you’re unsure, talk to your doctor about your full medication list.



Gabriella Adams
February 12, 2026 AT 23:38Okay, but can we talk about how wild it is that we’re still getting pamphlets in 2024 that say "antibiotics ruin birth control"? Like, the science has been clear for over a decade. I work in a pharmacy and I literally had a customer cry because she thought she was "going to get pregnant from amoxicillin." We need better education, not fear-based pamphlets.
Also, I love that you mentioned rifaximin. So many people panic about "rif-" drugs, but that one’s just a gut-only antibiotic. It’s literally designed not to interfere with systemic meds. Such a simple distinction, yet so many get it wrong.
And St. John’s Wort? Bro. That stuff is a silent killer for birth control. I had a friend on it for anxiety and got pregnant despite perfect pill use. She had no idea. No one tells you about herbal supplements. We need warning labels on those bottles too.
Why does this myth persist? Because it’s easier to say "just use condoms" than to explain pharmacokinetics. But we’re not doing anyone favors by oversimplifying. Women deserve accurate info. Not blanket warnings.
I’m so glad the FDA updated the labels. That’s huge. Now pharmacists can’t hide behind "we’ve always said this." Time to update the training modules. I’ve been pushing for it for years.
Also, if you miss a pill? That’s the real red flag. Not the antibiotic. But no one talks about that. We fixate on the wrong thing. Prioritize consistency over paranoia.
And for the love of all things medical - if you’re on lamotrigine or topiramate? Talk to your doctor. Don’t Google it. That’s how people end up in ERs.
Thanks for writing this. Someone needed to say it clearly.
Alyssa Williams
February 14, 2026 AT 02:09amoxicillin = fine. rifampin = bad. st johns wort = worse. that’s it. no drama. no panic. just take your pill.
Ernie Simsek
February 15, 2026 AT 11:51bro this is why I hate medical advice on the internet 😂
"antibiotics ruin birth control" - NOPE. "st john's wort is safe" - NOPE. "you’re fine" - YES. "your pharmacist is wrong" - YES.
I just got prescribed doxycycline for acne and my pharmacist handed me a condom. I said "I’m on the pill." She said "better safe." I said "I’m gonna cite the 2020 CDC study." She said "I’ll call my manager."
Then she gave me a free lube sample. I’m not mad. I’m impressed.
Also, if you’re on HIV meds and birth control? Yeah, you’re probably fine. But ask. Don’t assume. I learned this the hard way.
Also also - rifaximin is not rifampin. I’ve seen people panic about traveler’s diarrhea meds. It’s like confusing a firecracker with a nuke.
👏👏👏
Reggie McIntyre
February 16, 2026 AT 00:24This is the kind of post that makes me believe in humanity again.
I used to be one of those people who swore up and down that antibiotics ruined birth control. Then I read the studies. Then I talked to my OB-GYN. Then I realized I’d been living in a 1998 mindset while the world moved on.
It’s wild how much misinformation sticks. Like, I’ve seen TikTok videos where girls are showing their amoxicillin prescriptions and saying "I’m gonna be a mom now." No. You’re gonna be fine. Your body knows what it’s doing.
And St. John’s Wort? Oh man. That’s the sneaky one. I took it for mild depression and didn’t even know it was a drug interaction. I thought it was "natural" so it was safe. Nope. It’s basically a chemical grenade.
Also - why do we still let pharmacists hand out outdated pamphlets? They’re not trained in pharmacokinetics. They’re trained in insurance forms.
Can we make a petition to update all pharmacy handouts? I’ll start a GoFundMe. I’ll even design the new one. I’ve got a Canva Pro account.
Thank you for this. I’m sharing it with everyone I know.
Ojus Save
February 17, 2026 AT 07:39yea i read this and i was like oh ok so amoxicillin is fine but what about cipro? i think i read somewhere it might affect it? or was that the other one?
anyway thanks for clarifying
Jack Havard
February 17, 2026 AT 17:59So let me get this straight - you’re telling me the entire medical establishment got this wrong for 50 years, and now suddenly we’re supposed to believe a 2020 study? What about the 1970s case reports? What about the 2003 FDA advisory? What about the 12 women who got pregnant while on amoxicillin? You’re ignoring the anecdotal evidence.
Also, I’ve seen the CDC website. It says "may interact." "May" means uncertainty. You’re treating uncertainty like fact.
And why does the FDA update labels? Because of lawsuits. Not science. Always look at the motive.
I’m not saying you’re wrong. I’m saying you’re too confident.
Rachidi Toupé GAGNON
February 19, 2026 AT 00:23Yessssssssss 🙌
Finally. Someone said it without jargon.
Amoxicillin? Chill. Rifampin? Nuke it. St. John’s Wort? That’s a villain in a Marvel movie.
I’m telling my sister. She’s on the ring and just got a sinus infection. She’s about to panic. I’m sending her this.
Also - rifaximin ≠ rifampin. I’m writing that on my fridge.
Thank you.
Vamsi Krishna
February 20, 2026 AT 23:56You say "studies show" - but which studies? Are they funded by Big Pharma? Who wrote them? Were they peer-reviewed? Or just published in some pay-to-play journal?
I’ve been on birth control for 12 years. I’ve taken 17 courses of antibiotics. I’ve never missed a pill. And yet - I got pregnant once. It was right after a course of amoxicillin.
Coincidence? Maybe. But I don’t trust studies that say "no effect." I trust my body.
Also - why don’t you mention that birth control pills have a 9% failure rate anyway? That’s not because of antibiotics. That’s because of human error. So why blame the pill? Why not blame the user?
You’re just another influencer pushing a narrative.
christian jon
February 22, 2026 AT 13:21Okay, I’m done.
First - the FDA doesn’t care about you. They care about lawsuits. The "updated labels"? That’s because a woman sued after she got pregnant. Not because of science - because of money.
Second - your "2020 study"? That was funded by Pfizer. Who also makes birth control. Conflict of interest? Nope. Just coincidence.
Third - I’ve been on doxycycline for acne. My period stopped. I got a positive pregnancy test. I was on the pill. I didn’t miss a pill. I didn’t take St. John’s Wort. I didn’t take rifampin. So what happened?
Fourth - why is no one talking about the 100+ women who posted on Reddit saying they got pregnant on antibiotics? Are they all lying? Are they all "misinformed"?
Fifth - why are you so confident? Why aren’t you scared? Why aren’t you cautious? Why are you so eager to tell women they’re safe?
Sixth - what if you’re wrong?
Seventh - I’m not taking risks with my body.
Eighth - I’m using condoms. Always. Always. Always.
Ninth - I’m not your guinea pig.
Tenth - I’m not sharing this post.
Suzette Smith
February 24, 2026 AT 05:26I’m not saying you’re wrong - I’m just saying I’m not convinced.
I’ve read your studies. I’ve read the CDC. I’ve read the FDA.
But I’ve also read the 2018 study from the University of Texas that said amoxicillin *might* slightly reduce absorption in women with IBS.
And I’ve read the 2021 case report from the UK where a woman on amoxicillin got pregnant after vomiting.
So - maybe the risk is low. But is it zero?
And if it’s not zero… why take it?
I’ll keep using condoms. Just in case.
Not because I think it’s necessary.
Because I don’t want to argue about it later.
Pat Mun
February 24, 2026 AT 06:08Thank you for writing this. I’ve been waiting for someone to break this down clearly.
I’m 34, on the pill, and I’ve been prescribed antibiotics like amoxicillin and azithromycin at least six times over the last decade. I’ve never used backup. Never had a problem.
But I’ve also seen friends panic. One friend stopped her pill for two weeks because she got a UTI and was on cipro. She got pregnant. She thought it was the antibiotic. It was a missed pill. She forgot because she was sick.
Another friend took St. John’s Wort for anxiety and didn’t tell her doctor. She got pregnant. She didn’t know it interacted. She thought it was "natural."
And now I have a 19-year-old niece on the ring. She’s about to get amoxicillin for an ear infection. I’m sending her this.
I’m so tired of the fear. I’m so tired of the outdated advice. I’m so tired of women being talked down to.
This isn’t just about birth control. It’s about trust. Trust in science. Trust in your body. Trust in your doctor.
Please keep writing stuff like this.
Sophia Nelson
February 25, 2026 AT 18:57Okay, but what about the 2022 study that showed a 12% drop in hormone levels in women taking amoxicillin with high-fat meals? You didn’t mention that.
And what about the fact that the WHO says "consult your doctor"? That’s not a green light. That’s a warning.
Also - you say "no backup needed" - but what if you’re obese? What if you have liver disease? What if you’re on SSRIs? What if you’re over 35? What if you smoke?
There are so many variables. You’re oversimplifying.
And why isn’t there a pill that doesn’t interact with anything? Why do we have to do this math?
Why is birth control so complicated?
Why can’t we just have a pill that works?
Jason Pascoe
February 26, 2026 AT 14:46Just wanted to say - I’m from Australia and we’ve been on the same page here for years. Pharmacists here don’t hand out those pamphlets anymore. We updated our guidelines in 2019.
Also - rifaximin is called Xifaxan here too. No one confuses it with rifampin. We call rifampin "TB drug" and everyone knows.
St. John’s Wort? Yeah. We have a warning on the bottle. It’s mandatory.
So… maybe it’s not that the science is new.
Maybe it’s that the US is just… behind.
Just saying.
Sonja Stoces
February 27, 2026 AT 15:14So let me get this straight - you’re telling me I can take amoxicillin and not use condoms… but I can’t take St. John’s Wort?
That’s not a scientific distinction. That’s a cultural one.
One is a drug. One is a supplement.
One is regulated. One isn’t.
So what’s really going on here?
Are you just saying "pharmaceuticals are safe, herbs are dangerous"?
Or are you just scared of herbal medicine?
And why do we still have to worry about this at all?
Why isn’t there a birth control that doesn’t interact with ANYTHING?
Why are we still stuck in this 1970s system?
Why do we have to be so careful?
Why can’t we just be free?