Amiodarone Photosensitivity Risk Calculator
This tool estimates your risk of developing photosensitivity while taking amiodarone based on your dosage, treatment duration, and skin type. For medical advice, consult your physician.
Your Risk Assessment
Prevention Recommendations
Ever noticed a rash that flares up after a sunny walk while you’re on a heart medication? That could be amiodarone photosensitivity. Understanding why it happens, spotting the signs early, and taking simple steps to protect your skin can keep you safe without stopping a life‑saving drug.
What is Amiodarone‑Induced Photosensitivity?
Amiodarone is a Amiodarone is a class‑III antiarrhythmic medication used to control irregular heartbeats. It works by prolonging the cardiac action potential, helping to stabilize rhythm (especially in atrial fibrillation and ventricular tachycardia). When this drug interacts with sunlight, the skin can become unusually sensitive, a condition known as photosensitivity. In medical terms, Photosensitivity is an abnormal skin reaction that occurs after exposure to ultraviolet (UV) radiation, often appearing as redness, itching, or a burning sensation. This reaction isn’t an allergy; it’s a chemical‑induced amplification of the skin’s response to UV light.
How Does Amiodarone Cause Photosensitivity?
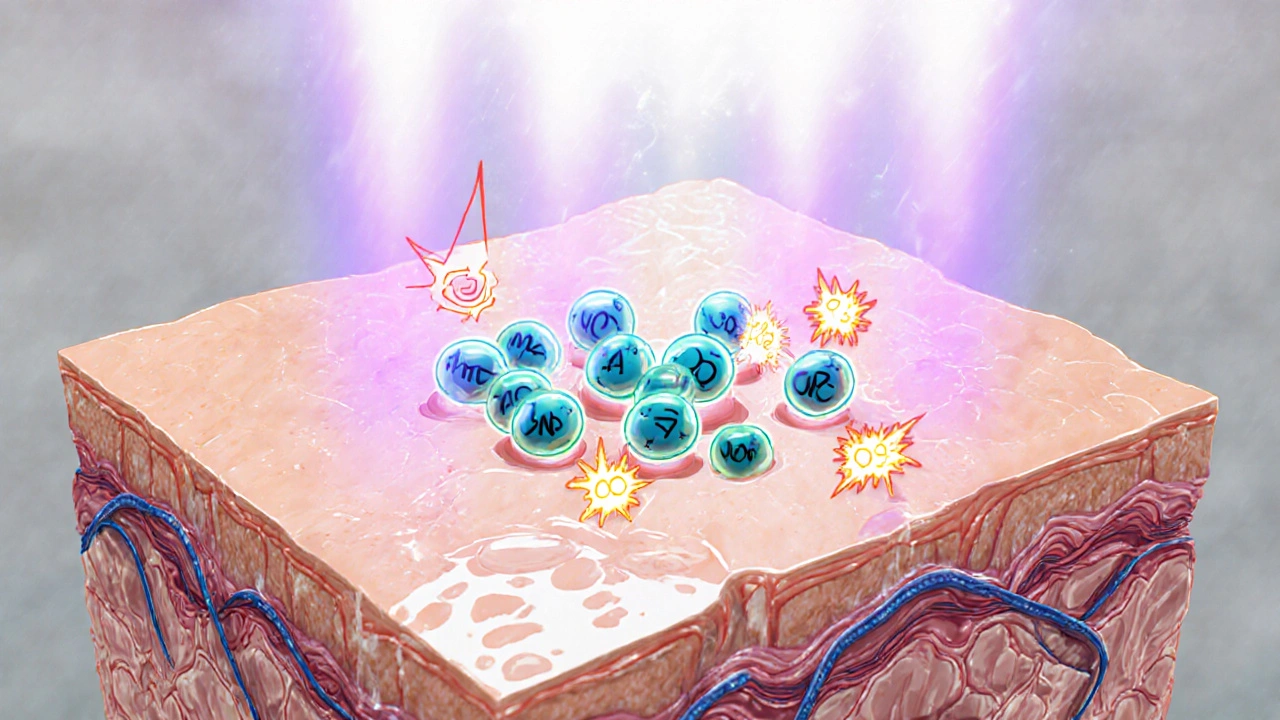
The exact pathway is still under study, but two main mechanisms are widely accepted:
- Drug accumulation in the skin: Amiodarone is lipophilic, meaning it dissolves in fats. Over weeks to months, it builds up in the dermis and epidermis, especially in sun‑exposed areas.
- Generation of reactive oxygen species (ROS): When the drug‑laden skin meets ultraviolet A (UVA) light, it can produce free radicals that damage cellular membranes, leading to inflammation.
UVA radiation, which penetrates deeper than UVB, is the primary culprit. UVA radiation has wavelengths between 320‑400nm and is present even on cloudy days, making it a silent trigger for photosensitive reactions.
Who Is Most at Risk?
Not everyone on amiodarone will develop a skin reaction, but several factors raise the odds:
- High cumulative dose: Doses above 400mg/day for longer than six months increase skin deposition.
- Geographic location: Living closer to the equator or spending lots of time outdoors raises UV exposure.
- Skin type: Fair‑skinned individuals (Fitzpatrick I-II) are more prone to UV‑induced damage.
- Concurrent medications: Drugs that also sensitize the skin (e.g., doxycycline, thiazides) can have an additive effect.
- Liver function: Impaired hepatic metabolism reduces the breakdown of amiodarone, leading to higher blood levels. The enzyme Cytochrome P450 (particularly CYP3A4) metabolizes amiodarone; liver disease or enzyme inhibitors can increase drug concentration.
Recognizing the Symptoms
Photosensitivity doesn’t always look the same. Common presentations include:
- Redness or a sunburn‑like rash on the face, neck, forearms, or hands.
- Itching or a burning sensation that intensifies a few hours after sun exposure.
- Hyperpigmentation (dark spots) that persist weeks after the initial flare.
- Peeling or flaking skin, especially after repeated exposure.
Because the reaction can mimic a simple sunburn, patients often attribute it to ordinary UV damage and miss the drug link. A key clue is the timing: the rash appears after a few weeks of stable amiodarone dosing, and it improves when the patient reduces sun exposure.
How Doctors Diagnose It
Diagnosis is mainly clinical, based on history and physical examination. Physicians may:
- Ask about medication history, focusing on amiodarone dose and duration.
- Note the distribution of the rash-usually confined to sun‑exposed areas.
- Perform a skin biopsy if the presentation is atypical; pathology often shows a lymphocytic infiltrate with pigment incontinence.
- Rule out other causes such as lupus erythematosus, porphyria, or contact dermatitis.
Blood tests aren’t diagnostic for photosensitivity, but checking liver enzymes and thyroid function is routine for amiodarone monitoring, as the drug also affects these organs.
Prevention Strategies
The best approach is to reduce UV exposure while staying on the medication. Key steps include:
- Sun avoidance during peak hours: Stay under shade between 10am and 4pm when UVA intensity peaks.
- Protective clothing: Wear long sleeves, wide‑brimmed hats, and UV‑blocking sunglasses.
- Use broad‑spectrum sunscreen: Choose a Sunscreen that blocks both UVA and UVB, with an SPF of at least 30. Apply 15minutes before heading outdoors and reapply every two hours.
- Consider dose adjustment: If photosensitivity becomes severe, physicians may lower the daily dose or switch to alternatives like dronedarone (which carries a lower skin‑reaction risk).
- Regular skin checks: Schedule dermatology appointments annually, especially for patients with a history of skin cancer.
Patients often wonder whether a higher‑SPF formula offers extra protection. While SPF mainly measures UVB blockage, the “broad‑spectrum” label ensures UVA coverage, which is the critical factor for amiodarone‑related reactions.
Managing an Acute Flare‑Up
If a rash does appear, prompt treatment can limit discomfort and prevent scarring:
- Cool compresses: Apply cool, damp cloths to soothe burning sensations.
- Topical corticosteroids: Low‑to‑moderate potency steroids (e.g., hydrocortisone 1%) reduce inflammation. Use for no more than two weeks to avoid skin thinning.
- Oral antihistamines: Non‑sedating options like cetirizine help control itching.
- Temporary photoprotection break: Limit sun exposure completely for a week, allowing the skin to recover.
- Medication review: Discuss with a cardiologist whether the amiodarone dose can be lowered or if an alternative antiarrhythmic is appropriate.
Never stop amiodarone abruptly without medical guidance; sudden discontinuation can trigger rebound arrhythmias.

Comparing Photosensitivity Risk Across Antiarrhythmic Drugs
| Drug | Class | Photosensitivity risk | Typical dose | Monitoring focus |
|---|---|---|---|---|
| Amiodarone | III | High | 200‑400mg/day | Liver, thyroid, skin |
| Dronedarone | III | Low | 400mg twice daily | Liver, renal |
| Sotalol | III | None reported | 80‑640mg/day | QT interval, renal |
| Flecainide | IC | None reported | 50‑300mg/day | ECG, renal |
The table shows that amiodarone carries a uniquely high risk. If a patient cannot tolerate strict photoprotection, clinicians often consider dronedarone or sotalol, which lack the photosensitivity issue.
Key Takeaways
Amiodarone saves lives by controlling dangerous heart rhythms, but its tendency to make skin overly sensitive to sunlight can be bothersome. Recognizing the early signs-redness, itching, and hyperpigmentation after sun exposure-is the first step. Consistent use of broad‑spectrum sunscreen, protective clothing, and timing outdoor activities can prevent most reactions. When a flare does occur, cool compresses, topical steroids, and a short break from UV exposure typically resolve the problem without stopping the medication. Always coordinate any dose changes with a cardiologist, as abrupt discontinuation can be hazardous.
Frequently Asked Questions
How long after starting amiodarone can photosensitivity appear?
Most patients notice skin changes within 2‑6weeks of a stable dose, but the reaction can take up to 3months as the drug builds up in the skin.
Can I use any sunscreen, or does it need to be special?
Choose a broad‑spectrum sunscreen that blocks both UVA and UVB, with an SPF of 30 or higher. Look for ingredients like zinc oxide or titanium dioxide, which reflect UVA effectively.
Is it safe to lower my amiodarone dose on my own if I get a rash?
No. Dose adjustments must be directed by a cardiologist, because reducing the dose too quickly can cause the arrhythmia to return.
Do other drugs cause similar skin reactions?
Yes. Tetracycline antibiotics, thiazide diuretics, and non‑steroidal anti‑inflammatory drugs (NSAIDs) can also trigger photosensitivity, but the mechanism differs from amiodarone’s.
Should I get regular skin checks while on amiodarone?
Annual dermatology exams are recommended, especially for fair‑skinned patients or those with a history of skin cancer.



Grace Hada
October 17, 2025 AT 21:11Amiodarone’s skin‑shimmer is just the heart’s way of demanding respect.
Nis Hansen
October 25, 2025 AT 04:23The guide correctly highlights the lipophilic nature of amiodarone, which explains its accumulation in dermal layers. UVA‑induced ROS generation is a plausible mechanistic pathway, aligning with oxidative stress literature. Patients should be counseled on broad‑spectrum sunscreen, as UVB‑only products miss the primary trigger. Moreover, interdisciplinary monitoring-cardiology and dermatology-optimizes outcomes.
Fabian Märkl
November 1, 2025 AT 10:35Great breakdown! I’ve seen a few folks forget to reapply sunscreen every two hours, and the rash can get nasty fast. Keep spreading the word, and don’t forget that a wide‑brimmed hat is a cheap, effective shield 😊
Avril Harrison
November 8, 2025 AT 17:47Interesting read. I’m from the UK, and we don’t get as much intense UVA, but I still see patients on amiodarone complaining about sun‑related skin issues. Maybe it’s worth reminding them that cloud cover isn’t an excuse.
Natala Storczyk
November 16, 2025 AT 00:59THIS IS NOT SOME TRIVIAL SUNBURN!!! THE DRUG IS A SERIOUS CHEMICAL THAT INSULTS YOUR SKIN!!! YOU MUST SLAP ON THE HIGHEST SPF AND NEVER STEP OUT DURING PEAK HOURS!!! IGNORE THIS AND YOU’LL END UP WITH PERMANENT DISCOLORATION AND SCAR‑RICH TRAGEDY!!!!
nitish sharma
November 23, 2025 AT 08:11The phenomenon of amiodarone‑induced photosensitivity warrants careful consideration by clinicians managing arrhythmic patients.
Amiodarone’s high lipophilicity facilitates its sequestration within the epidermal and dermal matrices over prolonged administration.
Consequently, ultraviolet A radiation interacts with the drug‑laden cutaneous tissue, provoking the formation of reactive oxygen species.
These photogenerated radicals initiate a cascade of inflammatory mediators, manifesting clinically as erythema, pruritus, and occasionally hyperpigmentation.
Epidemiological observations indicate that patients receiving daily doses exceeding four hundred milligrams for more than six months are at heightened risk.
Geographical latitude further modulates exposure, with equatorial regions delivering greater cumulative UVA fluence.
Furthermore, concurrent use of ancillary photosensitizing agents such as doxycycline or thiazide diuretics can exert additive effects.
Given the potential for misattribution to ordinary sunburn, a thorough medication history is indispensable during dermatologic assessment.
Diagnostic confirmation relies principally on temporal correlation rather than invasive procedures, although biopsy may be justified in atypical presentations.
Management strategies prioritize rigorous photoprotection, encompassing broad‑spectrum sunscreens with a minimum SPF of thirty, applied fifteen minutes before exposure.
Patients should be instructed to reapply the protective formulation at two‑hour intervals, especially after perspiration or aquatic activities.
Complementary measures include seeking shade during the peak intensity window of ten a.m. to four p.m., and donning protective clothing such as long sleeves and wide‑brimmed hats.
In cases of severe cutaneous reaction, low‑to‑moderate potency topical corticosteroids may be employed for a limited duration to mitigate inflammation.
Systemic antihistamines can address pruritic symptoms, while a temporary cessation of outdoor activities permits cutaneous recovery.
Any contemplated adjustment of amiodarone dosage must be coordinated with a cardiology specialist to avert rebound arrhythmias.
Finally, regular dermatologic surveillance, at least annually, is advisable for individuals with fair skin phenotypes or a prior history of cutaneous malignancy.
Rohit Sridhar
November 30, 2025 AT 15:23Nicely summarized! It's encouraging to see that simple habits-like choosing the right sunscreen and timing outdoor runs-can make a huge difference. Keep the optimism alive, and patients will feel empowered to stay protected.
Sarah Hanson
December 7, 2025 AT 22:35Thanks for the comprehensive guide; it’s really helpful for both clinicians and patients alike. Remember to reapply sunscreen-don’t skimp on that step, it’s definatly worth it.
Nhasala Joshi
December 15, 2025 AT 05:47Wake up, people! The pharma giants push amiodarone knowing it’ll turn your skin into a UV‑sensitive battlefield-an intentional side‑effect to keep you dependent on costly dermatologic treatments. The oxidative stress pathway is just a cover for their profit‑driven agenda, and the “broad‑spectrum” label is a marketing gimmick, not a shield. Stay vigilant, question the standard of care, and demand transparent research 🙈
kendra mukhia
December 22, 2025 AT 12:59Honestly, most of the advice you’ve seen online is superficial; the real issue is that clinicians often overlook the cumulative dose threshold. If you’re not monitoring amiodarone plasma levels, you’re setting your patients up for avoidable dermatologic complications.
Bethany Torkelson
December 29, 2025 AT 20:11Stop ignoring the sunscreen protocol-your skin will thank you.