Diabetes Alcohol Risk Calculator
Assess your personal risk based on your medications, drinking habits, and precautions
Drinking alcohol while taking diabetes meds isn’t just a bad idea-it can be dangerous. For people using insulin, sulfonylureas, or even metformin, alcohol doesn’t just add empty calories. It can trigger life-threatening low blood sugar, hide the warning signs, and strain your liver in ways you might not realize. And the worst part? Many people don’t know they’re at risk until it’s too late.
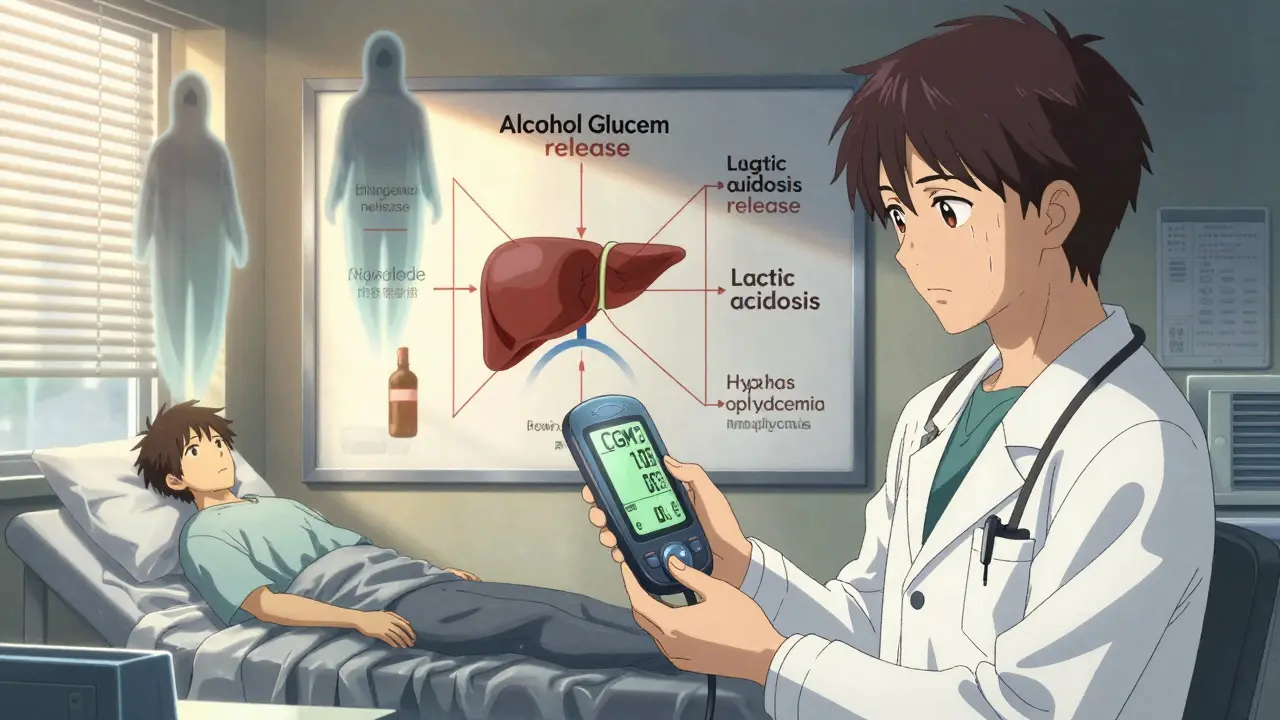
Why Alcohol Causes Low Blood Sugar
Your liver has two big jobs: storing and releasing glucose to keep your blood sugar steady, and breaking down alcohol. When you drink, your liver drops everything else to handle the alcohol. That means it stops releasing glucose into your bloodstream. If you’re on a medication that lowers blood sugar-like insulin or glipizide-that’s when things go wrong.Low blood sugar, or hypoglycemia, can hit fast. You might feel shaky, sweaty, dizzy, or confused. But here’s the trap: those symptoms look exactly like being drunk. Slurred speech, stumbling, drowsiness-doctors call this the alcohol-hypoglycemia mimic. If you pass out after a few drinks, someone might assume you’re just intoxicated. They might not check your blood sugar. And that delay can cost you your life.
And it’s not just while you’re drinking. Hypoglycemia can happen hours later, even overnight. That’s why so many people with diabetes wake up in the middle of the night with a pounding heart, drenched in sweat, or confused as hell. One Reddit user described checking their CGM at 3 a.m. after drinking wine with dinner: blood sugar at 48 mg/dL. They had no symptoms until then. That’s hypoglycemia unawareness in action.
Metformin and Alcohol: A Silent Strain
Metformin is one of the most common diabetes pills. It’s usually safe. But mix it with alcohol, and you’re asking for trouble. Both metformin and alcohol are processed by the liver. When you combine them, your liver gets overloaded. That increases your risk of lactic acidosis-a rare but deadly condition where lactic acid builds up in your blood. Symptoms? Nausea, vomiting, stomach pain, muscle cramps, rapid breathing. It’s easy to mistake for a bad hangover.And it’s not just about big drinking. Even a couple of beers or a glass of wine can worsen metformin’s usual side effects: bloating, gas, diarrhea, nausea. If you’re already feeling queasy from the pill, alcohol makes it worse. The more you drink, the higher the risk. And if you’ve got existing liver issues-say, from fatty liver disease, which is common in type 2 diabetes-you’re in even more danger.
How Alcohol Messes With Your Liver
Your liver doesn’t just handle sugar. It’s your body’s main detox center. Chronic alcohol use leads to inflammation, fat buildup, scarring-conditions like alcoholic hepatitis and cirrhosis. These aren’t just liver problems. They wreck your blood sugar control.When your liver is damaged, it can’t store glucose properly. That means your blood sugar swings wildly: too low after drinking, too high when you’re not. It also makes your body less responsive to insulin. So even if you’re taking meds, they stop working as well. Studies show people with diabetes who drink heavily have a 30% higher chance of developing advanced liver disease than those who don’t.
And here’s the kicker: alcohol affects the same liver enzymes (CYP2E1, CYP3A4) that break down many diabetes drugs. That means your body might process your meds slower-or faster-than normal. You could end up with too much drug in your system, or not enough. Either way, your blood sugar goes off track.

Which Medications Are Riskiest?
Not all diabetes meds carry the same risk. Here’s the breakdown:- Insulin and sulfonylureas (like glimepiride, glyburide): Highest risk. These force your body to release more insulin. Alcohol shuts down your liver’s glucose release. Double whammy. Hypoglycemia can happen fast and hard.
- Metformin: Lower hypoglycemia risk on its own, but alcohol increases chances of lactic acidosis and worsens GI side effects. Avoid heavy drinking.
- SGLT2 inhibitors (like empagliflozin, dapagliflozin): These cause sugar to spill out in urine. Alcohol can increase dehydration risk and raise the chance of ketoacidosis-even if your blood sugar isn’t high.
- DPP-4 inhibitors and GLP-1 agonists (like sitagliptin, semaglutide): Lower hypoglycemia risk. Still, alcohol can mask symptoms and worsen nausea.
If you’re on insulin or sulfonylureas, you’re in the danger zone. Even one drink can be risky if you’re not eating. The American Diabetes Association says there’s no universal safe amount. It depends on your meds, your liver, your eating habits, and whether you’ve lost the ability to feel low blood sugar coming.
How to Drink Safely (If You Choose To)
The truth? The safest choice is to skip alcohol. But if you decide to drink, here’s how to cut the risk:- Eat first. Never drink on an empty stomach. Have a meal or snack with carbs-whole grain toast, fruit, yogurt. This gives your liver something to work with besides alcohol.
- Choose wisely. Skip sugary cocktails, sweet wines, and regular beer. Opt for light beer, dry white wine, or spirits with soda water and lime. Avoid juice mixers-they spike your sugar.
- Limit the amount. Stick to one drink for women, two for men. That’s it. More than that? You’re increasing liver stress and hypoglycemia risk dramatically.
- Check your blood sugar. Test before you drink. Test again every 1-2 hours while drinking. Test before bed. If it’s below 100 mg/dL, eat a snack. Don’t wait until you feel symptoms.
- Wear medical ID. A bracelet or necklace that says “Diabetic” could save your life if you pass out.
- Tell someone. Make sure a friend or family member knows you have diabetes. Teach them how to recognize low blood sugar and how to give you glucose gel or juice.
And never drink if your blood sugar is already low, if you’re sick, or if you’ve been exercising hard. Exercise lowers blood sugar. Alcohol lowers it more. That combo is a recipe for disaster.
What the Experts Say
The American Diabetes Association doesn’t say “never drink.” They say: talk to your doctor. Your meds, your liver health, your history of low blood sugar-these all matter. A 2023 ADA guideline update now explicitly tells providers to ask patients about alcohol use during every visit. But here’s the problem: only 43% of primary care doctors actually do it.Diabetes educators are better. 89% of certified diabetes care specialists now include alcohol in their patient education. But if your doctor doesn’t bring it up, you need to. Ask: “Is it safe for me to drink with my current meds?” Don’t assume it’s fine.
Real Stories, Real Risks
One man in Sydney, 58, took metformin and had two glasses of wine with dinner. He felt fine. Went to bed. Woke up at 4 a.m. confused, sweating, heart racing. His CGM showed 39 mg/dL. He didn’t feel the usual warning signs. His wife found him slumped over. He ended up in the ER. No one knew he had diabetes.A woman in Melbourne drank a single cocktail with her husband after dinner. She took her evening insulin. She didn’t eat carbs. She woke up at 3 a.m. with a seizure. Her husband called an ambulance. Her blood sugar was 28 mg/dL. She spent three days in the hospital.
These aren’t rare. They happen every week. And they’re preventable.
What’s New in 2026
New CGM devices like the Dexcom G7 and FreeStyle Libre 3 now track patterns that might signal alcohol-related drops. They can’t detect alcohol directly, but they can show unusual overnight lows that don’t match your food or insulin. Some apps now let you log drinks and get alerts if your pattern matches past hypoglycemic events.Researchers at Joslin Diabetes Center are testing AI tools that predict your personal risk based on your meds, drinking habits, liver enzymes, and sleep patterns. Early results show they can flag high-risk days with 85% accuracy. This tech won’t be in your phone yet-but it’s coming.
The message is clear: alcohol and diabetes meds don’t mix well. Even moderate drinking carries hidden dangers. Your liver is already working hard. Don’t make it fight harder.
Can I drink alcohol if I have type 2 diabetes and take metformin?
You can, but with serious caution. Metformin and alcohol together increase the risk of lactic acidosis-a rare but life-threatening condition. Even one or two drinks can worsen nausea, vomiting, and stomach pain. Always eat food before drinking, avoid binge drinking, and never drink if you’re sick or have liver problems. Talk to your doctor about your personal risk.
Why does alcohol cause low blood sugar hours after drinking?
Your liver prioritizes clearing alcohol over releasing glucose. This effect lasts for several hours-even after you’ve stopped drinking. If you’re on insulin or sulfonylureas, your body keeps making insulin while your liver won’t release sugar. That’s why low blood sugar often hits at night or the next morning. Checking your blood sugar before bed and setting an alarm to check again can prevent emergencies.
What’s the safest type of alcohol for someone with diabetes?
The safest choices are low-sugar options: dry white wine, light beer, or spirits like vodka or gin mixed with soda water and lime. Avoid sweet cocktails, regular beer, dessert wines, and sugary mixers like juice or tonic water. These spike your blood sugar first, then crash it later when alcohol kicks in.
Can alcohol make my diabetes worse over time?
Yes. Heavy drinking (more than 15 drinks a week for men, 8 for women) damages your liver and pancreas. That makes it harder for your body to control blood sugar. It can lead to insulin resistance, fatty liver disease, and even worsen nerve damage from diabetes. Even moderate drinking can interfere with medication effectiveness and increase your risk of hypoglycemia.
What should I do if I think I’m having low blood sugar after drinking?
Don’t wait for symptoms to get worse. Test your blood sugar immediately. If it’s below 70 mg/dL, treat it with 15 grams of fast-acting carbs-like 4 ounces of juice, 3-4 glucose tablets, or 1 tablespoon of sugar. Wait 15 minutes, then test again. If it’s still low, treat again. Never assume you’re just drunk. If you’re confused, unconscious, or having a seizure, call emergency services right away.
Should I stop drinking completely if I’m on insulin?
Many people on insulin choose to avoid alcohol entirely because the risk of severe hypoglycemia is high-and it’s hard to predict. If you do drink, you must eat, monitor closely, and never drink alone. Talk to your diabetes care team. For some, the safest answer is no. For others, one drink with food might be manageable. It depends on your individual health, not a general rule.



Kathy Scaman
January 27, 2026 AT 20:17Just had a glass of wine with dinner and checked my CGM-68 mg/dL. I eat before drinking now. No more guessing.
Thanks for the reminder.
Mindee Coulter
January 29, 2026 AT 09:27My mom passed out after one glass of wine and they thought she was drunk. She had diabetes. No one knew. She spent a week in the hospital. This isn’t theoretical. It’s real.
Always wear your medical ID.
Lance Long
January 31, 2026 AT 00:39I used to think alcohol was just calories and a good time. Then I got diagnosed with type 2 and started on metformin. One beer and I felt like I was going to die. Nausea, sweating, shaking-like a bad hangover but worse.
Turns out it was lactic acidosis warning signs. I haven’t touched alcohol since. Best decision I ever made.
Don’t wait until it’s too late to listen to your body.
fiona vaz
January 31, 2026 AT 10:58For anyone on SGLT2 inhibitors-this is critical. I had ketoacidosis after a single cocktail. Blood sugar was normal. No warning. Just extreme fatigue and rapid breathing. ER visit. ICU. It’s not just about low blood sugar.
Alcohol messes with ketones too. Read the fine print on your meds.
Rose Palmer
February 1, 2026 AT 09:03As a certified diabetes care specialist, I’ve seen this too many times. Patients assume their doctor knows they drink. Doctors assume patients know the risks. The gap is deadly.
Every patient I see gets the alcohol conversation-no exceptions. If your provider doesn’t bring it up, ask. You deserve that level of care.
And yes, it’s okay to say no. Your liver will thank you.
Bryan Fracchia
February 2, 2026 AT 08:09Look, I get it. Life’s short. A glass of wine on Friday is part of my routine. But I’ve changed how I do it. Eat first. Stick to one. Check my glucose before bed. Tell my partner. Wear my bracelet.
It’s not about giving up joy. It’s about protecting your future.
You can still have a good time. Just don’t let it cost you your health.
Sue Latham
February 4, 2026 AT 05:44Ugh. People who say "just one drink" are delusional. You think you’re being responsible? You’re just one bad night away from an ambulance ride.
And if you’re on insulin? Please. Just don’t.
I’ve seen too many people ruin their lives over "a little fun."
Howard Esakov
February 5, 2026 AT 13:20Wow. So many people treat this like a hobby. 🤦♂️
Alcohol is a toxin. Your liver is already compromised. Your pancreas is crying. You’re on meds that are already taxing your system.
Do you really need to add a 500-year-old poison to the mix?
Just say no. It’s not even a question.
John Rose
February 6, 2026 AT 16:46Interesting that the 2026 AI tools are being tested. I wonder if they’ll integrate with Apple Health or Google Fit. If this tech can predict personal risk based on sleep, meds, and drinking patterns, it could be a game-changer.
But until then-stick to the basics: eat, monitor, communicate. No shortcuts.